INTRODUCTION
The endoscopic endonasal approach (EEA) to anterior cranial base pathology, such as olfactory groove meningiomas, has been well-described. EEA offers many advantages over open techniques, including panoramic view and direct access without the need for brain retraction, no external incisions, and the ability to devascularize lesions. Drawbacks may include alteration of olfactory function, nasal crusting, and risk of cerebrospinal fluid leak. Limitations of access, particularly for transplanum or transcribriform modules, include lateral extension beyond the internal carotid artery or mid-orbital roof (Future Neurol. 2012;7:263-277; Neurosurg Focus. 2014;37:E8) (Figure 1).
Explore This Issue
December 2022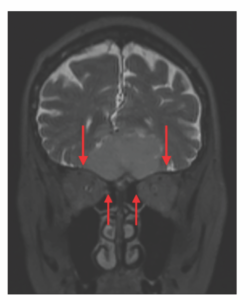
Figure 1. Coronal magnetic resonance imaging (MRI) demonstrating the lateral extent of the tumor (long arrows) compared to the medial orbit (short arrows).
We present a case of EEA for resection of a large olfactory groove meningioma in a 70-year-old female. The tumor was identified on imaging as part of a workup for altered mental status and falls. There was noted to be significant lateral extension of the tumor beyond the midorbital roof. In particular, we highlight the role of endoscopic medial and superior orbitotomy to allow for lateral supraorbital access and complete resection. This technique may help to further expand the role of EEA for experienced skull-base teams.
METHOD
Imaging, consisting of computed tomography and magnetic resonance imaging (MRI), should be carefully reviewed preoperatively. The extension of tumors in all directions and encasement of any critical neurovascular structures should be assessed. For the transcribriform and transplanum approaches, particular attention should also be paid to the location of the anterior and posterior ethmoid arteries, as these structures will be encountered and divided. Consideration should be given to the likely skull base defect and available reconstructive methods to prevent postoperative cerebrospinal fluid leak.
In the case of our patient, the procedure begins with the harvest of an extended nasoseptal flap for skull base reconstruction. Harvesting of the flap at the beginning allows it to be protected in the nasopharynx through the rest of the procedure and also facilitates nasal septectomy for access to the anterior cranial base. A second nasal septal flap can also be harvested from the contralateral septum as long as approximately 1 cm of caudal septal mucosa is preserved for structural support. This smaller flap can also be used in reconstruction or laid over the contralateral exposed nasal floor donor site of the extended flap.
Bilateral endoscopic sinus surgery is performed for exposure. Given the anterior extent of this tumor at the cribriform plate and its close proximity to the frontal sinus, we elected to perform an endoscopic modified Lothrop frontal sinusotomy to allow full access to the cribrito form and prevent postoperative frontal sinus stenosis. In cases of more posteriorly located tumors, the endoscopic modified Lothrop frontal sinusotomy may not be warranted. The bony nasal septum underlying the tumor is then removed. The anterior ethmoid artery is identified bilaterally and its relation to the orbit and skull base is noted.
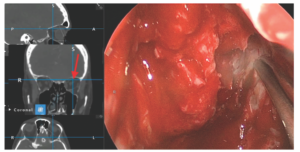
Figure 2. Endoscopic view with image guidance showing superolateral location of probe past the midpoint of the orbital roof.
For lateral supraorbital access, the lamina papyracea is carefully fractured away from the underlying periorbita. For anterior ethmoid arteries in close proximity to the skull base, removal of the lamina papyracea facilitates access so that the vessel can be controlled and divided. The posterior ethmoid arteries, sometimes with multiple branches, can also be controlled in a similar manner if encountered. The orbital contents can then be gently compressed, allowing superolateral access (Figure 2). All efforts should be made to keep the periorbita intact. Using a high-speed drill, skull base osteotomies can then be made at the appropriate location. Image-guidance software is helpful in this regard.
Once circumferential osteotomies are performed, dural incisions can be made and tumor removal can commence. Multi-layered skull base reconstruction followed by the vascularized extended nasoseptal flap is then performed.
RESULTS
The patient did well postoperatively, with improvement in her mental status. There were no orbital complications. Postoperative MRI demonstrated gross total resection.