 TRIO Best Practice articles are brief, structured reviews designed to provide the busy clinician with a handy outline and reference for day-to-day clinical decision making. The ENTtoday summaries below include the Background and Best Practice sections of the original article. To view the complete Laryngoscope articles free of charge, visit Laryngoscope.
TRIO Best Practice articles are brief, structured reviews designed to provide the busy clinician with a handy outline and reference for day-to-day clinical decision making. The ENTtoday summaries below include the Background and Best Practice sections of the original article. To view the complete Laryngoscope articles free of charge, visit Laryngoscope.
Explore This Issue
October 2018Background
Drooling, or sialorrhea, is a common problem among patients with cerebral palsy. The prevalence ranges from 37% to 58%. Drooling occurs when an individual’s ability to control and swallow oral secretions is limited. Common contributing factors include poor oropharyngeal coordination; dysphagia; poor posture or head position; dental abnormalities including malocclusion, nasal, or oropharyngeal obstruction; and gastroesophageal reflux. Patients may present with anterior drooling, posterior drooling, or both. Anterior drooling is defined as saliva spilled from the mouth that is clearly visible. This can have a significant medical and psychosocial impact on our patients and their families, including social rejection, damage to personal belongings, social isolation, frequent damp clothing, local skin irritation, and halitosis. Patients with posterior drooling, which occurs when saliva spills through the oropharynx and into the hypopharynx, can have serious medical consequences, including chronic aspiration leading to progressive lung disease.
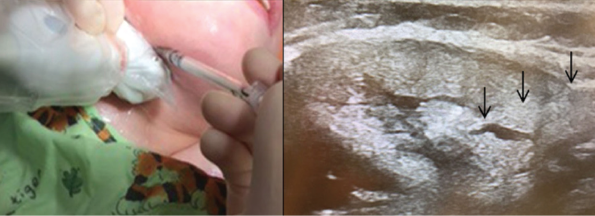
Botulinum toxin A injection into the right submandibular gland under ultrasound guidance. Positioning of the ultrasound probe in the submandibular region (left) and ultrasound image of the Botox injection with the black arrows highlighting the tract of the needle as it enters the submandibular gland (right).
© Copyright 2017 The American Laryngological, Rhinological and Otological Society, Inc.
Multiple interventions aimed at reducing or eliminating drooling have been described. These include physical and behavioral therapies, oral appliances, medications, botulinum toxin injections, and surgery. To date, there has been no clear consensus on which treatments of drooling are the safest and most effective. The goal of this review is to determine the role of botulinum toxin injections in the management of pediatric sialorrhea.
Best Practice
The published data on sialorrhea management is limited for all interventions, yet current literature supports the use of botulinum toxin injections as part of a therapeutic regimen. We are unable to conclude that botulinum toxin injections should be offered in lieu of anticholinergic medications; however, the CCT published by Jongerius et al. demonstrated a significant decrease in sialorrhea with both interventions but a more favorable side-effect profile for injections. This suggests that botulinum toxin injection may be ideal, especially for patients who are candidates for injections under local anesthesia. In patients who fail to improve following botulinum toxin, surgical intervention may be warranted (Laryngoscope. 2018;128:1259–1260).