VANCOUVER—The number of skin cancer cases in the U.S. is growing, and a huge number of those patients are treated with Mohs microsurgery, often performed by dermatologists. But a panel of head and neck surgery experts at the 2013 AAH-HNS Annual Meeting said that there are times when Mohs surgery might not be appropriate and that it’s a procedure that can come with down sides.
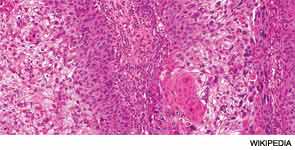
There has been a nearly 250 percent increase in procedures performed for skin cancer, paralleled by a rise in treatment of the disease by dermatologists, primarily through procedures performed in their offices, said Christine Gourin, MD, MPH, the session moderator and associate professor of otolaryngology-head and neck surgery at Johns Hopkins University in Baltimore. “Primarily, this treatment is Mohs,” she said. The microsurgery approach has been embraced because it spares healthy tissue while eradicating cancerous tissue, due to examination of the tissue during the procedure rather than afterward.
“The difficulty,” Dr. Gourin said, “is that dermatologists do not read the same literature that we do.” An example is literature acknowledging that the value of sentinel lymph node (SLN) biopsy is supported by evidence. “[Dermatologists] don’t see it as the standard of care,” she said.
Divide in Care Approach
Derrick Lin, MD, co-director of the Cranial Base Center at the Massachusetts Eye and Ear Infirmary in Boston, discussed the difference in approach between the head and neck surgery community and the dermatological community. “That’s always a tough question.… Most head and neck surgeons [will] say, ‘Well, Mohs is never indicated.’ You talk to a dermatologist, and they’ll say it’s indicated for everything. So, it’s always a hard divide between the two subspecialties.”
The dermatology literature says that resection without Mohs encompasses only 60 percent of margins, while Mohs encompasses the entire margin, accounting for its growth in popularity.
The degree to which the dermatology community has embraced Mohs surgery, he said, can be seen in a statement issued in 2012 by a consensus group of dermatologic surgeons. The group looked at 161 primary articles from the previous 71 years, case series of more than three and case reports. They tabulated the data and held four rounds of discussion.
The result is a report that concludes that Mohs is seen as “almost appropriate for everything,” Dr. Lin said. Both in and outside of the “H zone,” the area of the face that is considered at higher risk, the only situation deemed inappropriate for Mohs was primary or recurrent actinic keratosis with squamous cell carcinoma in situ.
There are certain large tumors where it is clear that Mohs is not appropriate, Dr. Lin said. He said the Mohs approach should be avoided in the setting of “extensive” lesions involving deep structures and in the setting of invasive melanoma, except with lentigo melanoma and in situ melanoma.
Sentinel Lymph Node Biopsy
Cecelia Schmalbach, MD, MS, co-director of the University of Alabama at Birmingham’s Cutaneous Head and Neck Oncology Board, said SLN biopsy is crucial in finding occult disease. It’s a minimally invasive technique to identify the “first echelon” lymph nodes that are mostly likely to harbor occult nodal metastasis.
She emphasized that it is only a staging tool, though, helping to identify who might benefit from adjuvant therapy and to spare patients without nodal disease the morbidity of a formal neck dissection. She noted that more data is needed to determine whether it’s actually therapeutic or could impact survival.
If a patient has a negative SLN biopsy, the current National Comprehensive Cancer Network guidelines say, there’s no need for formal neck dissection, but the patient should be followed clinically. “This is important, because anywhere on the order of 4 to 8 percent of patients will develop a second melanoma and that could be as late as 10 years out from their initial treatment,” she said. SLN for squamous cell carcinoma hasn’t yet been established, but she said that the data so far is “encouraging.”
Carol Bradford, MD, chair of otolaryngology at the University of Michigan, said the issue of whether or not to treat using the Mohs approach is crucial. “We have to consider how we are going to address the neck early enough in all of these patients such that the patients don’t suffer poor outcome due to regional failure,” she added. “Obviously, if patients have had a wide excision by the Mohs surgeon, the opportunity to do any sentinel lymph node biopsy to stage the regional nodal basin is gone.”
Cases of high-risk squamous cell carcinoma patients present a special challenge. “We can watch and wait, but we do know that that’s not a very effective strategy for picking up regional disease early enough to not have it be a big problem,” said Dr. Bradford. “I encourage you to consider strategies at the outset as to how to manage that regional basin.”
As for other malignancy types, serial sectioning and immunostaining are important for detecting small tumor burdens in sentinel nodes.
Neck dissection for N-positive disease must sacrifice involved structures as needed to eradicate the disease, even if that sometimes means facial nerves, said Dr. Bradford. Patient counseling should cover this possibility, as well as the potential need to do a mastoidectomy or resection of the lateral temporal bone. Immediate facial reanimation and soft tissue reconstruction should be considered, she said.
Other Treatments
Randal Weber, MD, FACS, chair of head and neck surgery at The University of Texas at MD Anderson Cancer Center in Houston, said surgery alone is usually adequate for early-stage skin cancer without aggressive features. But radiation therapy should be considered when there are positive margins or tumors larger than 4 cm with deep invasion, perineural invasion and lymph node metastasis.
POST (Post-Operative Skin Trial), an Australian trial, is looking at radiation alone versus radiation and chemotherapy in high-risk squamous cell patients, and Dr. Weber said he’s eagerly anticipating the results. “Look out for this study,” Dr. Weber said. “I think it’ll answer an important question, if we should intensify treatment for these very-high risk patients.”
Researchers at MD Anderson are also looking at the effectiveness of gefitinib in aggressive cutaneous squamous cell carcinoma cases. The drug, used in lung cancer patients for whom chemotherapy has failed, inhibits the activity of epithelial growth factor receptor, which is highly expressed in the skin. In a phase II study, patients were given the drug before standard therapy with surgery and/or radiation therapy. Three of 22 evaluable patients had a complete response, seven had a partial response and five were stable, Dr. Weber said. (Clin Cancer Res. 2012;18:1435-1446).
No biological basis has been found yet for the responders but studies are continuing. Dr. Weber said it might be a look at future treatments. “It’s pretty remarkable to think you can take one pill a day and get this sort of response from a skin cancer, especially an aggressive one.”
Leave a Reply