Does delaying surgical drainage in deep neck abscesses negatively affect outcome in adult and pediatric patients?
Bottom line: In adults, delay in surgical drainage of deep neck abscess is associated with increased morbidity and mortality (M&M), but there is no association between timing of drainage and M&M in children.
Explore This Issue
August 2016Background: Convention dictates that deep neck abscesses in adults require surgical drainage on an urgent basis, but there is limited evidence basis, and urgent surgical treatment versus conservative treatment for children has long been debated. It is unknown whether delaying drainage during a trial of conservative treatment increases the chances of potential spread of infection.
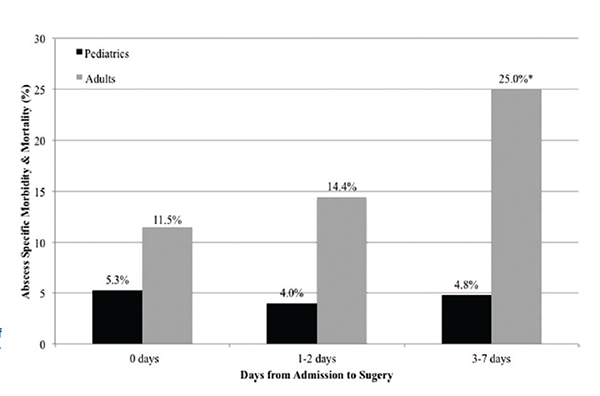
Primary outcome rate of abscess-specific morbidity and mortality by timing of surger
Copyright The American Laryngological, Rhinological and Otological Society, Inc
Study design: Multicenter, prospective, risk-adjusted cohort study of adult (n=347) and pediatric (n=665) patients with deep neck abscess who received incision and drainage within seven days of admission in the American College of Surgeons National Surgical Quality Improvement Program from 2005 to 2013 (adults) and from 2012 to 2013 (pediatrics).
Setting: American College of Surgeons National Surgical Quality Improvement Program and its companion pediatric database, ACS NSQIP Pediatric.
Synopsis: In adult patients, there was a significant increase in abscess-specific M&M with delay; postoperative septic shock, unplanned intubation or prolonged ventilation rate, and increased length of stay were significantly more likely. There was a significant increase in length of hospital stay for pediatric patients undergoing surgical drainage on days three to seven after admission; there were also no significant differences between groups for abscess-specific and nonspecific complications. Delay in surgical drainage significantly increased M&M rate for adult patients who received surgery three to seven days after admission. On multivariate regression, surgery timing, female gender, ASA [American Society of Anesthesiologists Physical Status Classification System] class III–V, preoperative sepsis or septic shock, and preoperative white blood cell count were significant postoperative M&M predictors in adults; in pediatrics, significant predictors were female gender, congenital malformation, ASA class III or IV, and preoperative sepsis or septic shock. In pediatric patients, congenital heart disease and ASA class III–IV were significant predictors of abscess-specific M&M. Limitations included possible errors or inconsistencies in coding, potential for selection bias, and several relevant variables omitted from data sources.
Citation: Cramer JD, Purkey MR, Smith SS, Schroeder JW Jr. The impact of delayed surgical drainage of deep neck abscesses in adult and pediatric populations. Laryngoscope. 2016;126:1753-1760.