Explore This Issue
February 2012Diagnosis: Killian-Jamieson diverticulum. The black arrow on the spot film shows a prominent cricopharyngeal muscle and the white arrow is the diverticulum.
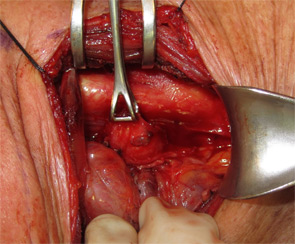
Management: The patient was taken to the operating room, esophagoscopy was performed and a nasogastric tube was placed in the esophagus to facilitate identification. The diverticulum was approached through a low left transcervical incision. The thyroid gland was retracted medially and the carotid sheath contents were retracted laterally, exposing the diverticulum. The diverticulum originated from the left lateral wall of the esophagus. The sac was intimately associated with the recurrent laryngeal nerve, which was identified, gently dissected off the sac and preserved (Figure 3). Diverticulectomy was performed, followed by esophagomyotomy and a two-layered closure. A drain was placed and the patient kept NPO for five days and then started on a clear liquid diet. At three weeks follow-up, the patient was tolerating a regular diet and reported complete resolution of symptoms. Repeat MBS did not identify any stricture.
Discussion: Killian-Jamieson diverticula represent a different type of diverticula than the more commonly diagnosed Zenker’s diverticula. Although both diverticula occur at sites of weakness in the cervical esophagus, there are important anatomical differences. Killian-Jamieson diverticula originate from the lateral wall of the pharyngoesophageal junction in the space below the cricopharyngeus muscle and lateral to the longitudinal muscular fiber of the esophagus, corresponding to a muscular gap where the recurrent laryngeal nerve enters the larynx (Killian-Jamieson’s space). Zenker’s diverticula originate from the posterior wall of the pharyngoesophageal junction below the superior constrictor muscle and above the cricopharyngeus muscle (Killian’s dehiscence).
Killian-Jamieson diverticula are intimately associated with the recurrent laryngeal nerve as it enters into the larynx. Inappropriate constriction of the circular muscle fibers of the proximal esophagus with normal cricopharyngeus function are presumed to result in high pressures, resulting in herniation of the esophageal mucosa below the cricopharyngeus in Killian-Jamieson diverticula. Improper relaxation of the cricopharyngeus muscle causes herniation of the esophageal mucosa above the cricopharyngeus and below the inferior pharyngeal constrictors superiorly in Zenker’s diverticula. Identification of the cricopharyngeal bar on MBS is critical in differentiating the two entities. The majority of patients with Killian-Jamieson diverticula are asymptomatic, and intact cricopharyngeal function is likely the reason for the absence of aspiration in Killian-Jamieson patients, in contrast with patients diagnosed with Zenker’s diverticula.
Patients with Killian-Jamieson diverticula are typically older than patients with Zenker’s diverticula by approximately 10 years, and Killian-Jamieson sacs are usually smaller than those found in Zenker’s diverticula. While the majority of patients with Killian-Jamieson diverticula are asymptomatic, surgery is indicated for symptomatic cases. Knowledge of the relationship of Killian-Jamieson diverticula to the recurrent laryngeal nerve is essential for nerve identification and preservation at surgery. In contrast to Zenker’s diverticula, cricopharyngeal myotomy is not indicated in the treatment of Killian-Jamieson diverticula, the formation of which the circular esophageal muscle inferior to the cricopharyngeus may cause.
Leave a Reply