Match Day has its traditions: Amid the pop of champagne corks, medical students across the country simultaneously open their envelopes to learn where they’ll spend their next few years as medical residents.
Explore This Issue
June 2018Traditionally, otolaryngology has been a much sought-after specialty. In 2014, however, the number of otolaryngology Electronic Residency Application Service (ERAS) applications began to drop; in 2017, the number
of ranked U.S. seniors who applied to the specialty (303) fell below the actual number of available positions (305), and 14 spots went unfilled after the initial match—unprecedented in recent otolaryngology matches, said David Chang, MD, residency program director and Jerry W. Templer, MD Faculty Scholar in Otolaryngology and associate professor of clinical otolaryngology at the University of Missouri in St. Louis (see Figure 1).
This year’s match didn’t fare much better, according to Dr. Chang, who collected data on match statistics: The number of ranked U.S. seniors (299) again fell below the actual number of available positions (312). And, while four more resident spots were filled in 2018 than in 2017, those additions didn’t offset the seven additional residency openings available this year.
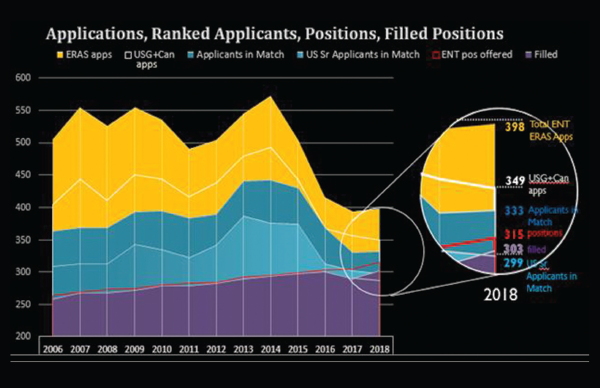
Figure 1. Otolaryngology Residency Applications, Ranked Applications, Positions, Filled Positions.
Note: ERAS application numbers are taken from data published in February of each match year, and do not include SOAP applications.
Reprinted with permission from David Chang, MD
“We’re the only surgical subspecialty that has noticed this down trend in total applications over the last two years,” said Stacey Gray, MD, program director for the Harvard Medical School otolaryngology program and current chair of the Otolaryngology Program Directors Organization (OPDO). “Harvard didn’t have any medical students who applied to otolaryngology in the last two years; I’ve been here since 1999 and that’s never happened before. However, if you look back even further the number of applications was trending down after a very significant peak in applications, with something like a 20% non-match rate probably four to five years ago.”
Although the numbers are certainly interesting (and some say possibly alarming), the question is why residency positions are going unmatched.
Why the Drop?
There are several potential issues upon which most program directors and residency advocates agree—with the caveat that the data don’t show a clear cause:
Work/life balance. Charles Elmaraghy, MD, chief of the department of otolaryngology at Nationwide Children’s Hospital and an assistant professor of clinical otolaryngology at The Ohio State University College of Medicine in Columbus, believes that work/life balance is a priority for current medical students. “We see students with an initial interest in otolaryngology switch to less-demanding nonsurgical specialties because they want to have a ‘normal’ family life rather than the long work hours that are inherent in a surgical specialty.”
Dr. Chang agreed, noting that urology, another surgical specialty, had a less dramatic version of otolaryngology’s match problem this year. “Surgical specialties are a little more unpredictable in work days and calls to emergency cases than other, nonsurgical, specialties like ER, radiology, and dermatology.”
Ksenia Aaron, MD, a neurotologist fellow at Stanford University in California and a recent graduate from the Keck School of Medicine at the University of Southern California in Los Angeles, found that some students in her rotation who initially pursued otolaryngology moved to different specialties. “When I’d follow up and see where they matched, at least 20% went on to a completely different subspecialty,” she said. “Being in surgery sometimes 12 to 14 hours might not fit what they envisioned.”
Loss of otolaryngology curriculum. Many program directors believe that students may not be exposed to otolaryngology due to a lessening of the specialty’s presence in current medical school curriculum. “Otolaryngology has been taken out of the curriculum at Ohio State,” said Dr. Elmaraghy. “It had been reduced over the last several years, and we noticed a reciprocal decline in students being interested in the field.”
“Otolaryngology is a fairly small, very specialized field,” agreed Dr. Gray. “If students don’t get that exposure, especially early on during the first and second years of medical school, then by the time they’re preparing for the match they’re missing a lot of components.”
“It’s impossible to match in otolaryngology.” Another concern is whether the selectiveness of otolaryngology programs actually dissuades some students from applying. “Until just a few years ago, we were suggesting that program directors be more honest if they thought applicants didn’t have a strong application,” said Barry Schaitkin, MD, chair-elect of the OPDO and professor and residency program director at the University of Pittsburgh, whose program didn’t fill its quota this year for the first time. “So we started putting out the message that otolaryngology was a specialty that’s very hard to get into, and if your application didn’t have certain accolades, it put you at risk for not matching.”
“As a third-year medical student, it was extremely daunting to look at the average scores and the match rate,” said David R. Lee, MD, a PGY-3 resident at the University of Cincinnati department of otolaryngology–head and neck surgery who participated in the 2015 match. “The attendings who told medical students to not apply to ENT were just looking out for their students’ best interests, because to not match is a terrible thing—you’ve gone through four years of medical school, and then you don’t have a job.”
Applying to too many programs. According to Dr. Aaron, the current philosophy for students is to “apply a lot, apply broadly, and keep what you get.” Unfortunately, this can put some students at a disadvantage to match. “More students are being encouraged to apply to 60 to 80 programs, rather than their top 20 or 30,” she said. (Per Dr. Chang, in 2015, applicants submitted a mean all-time high of 64.5 applications per applicant, the equivalent of applying to 60% of otolaryngology programs.) “So a select few applicants go to their top choices, but the other choices they selected don’t get the opportunity to interview applicants who could have potentially matched.”
Additional requirements for otolaryngology applicants. To try to encourage selectivity among applicants, otolaryngology added other requirements, including a customized personal statement paragraph for each program (now optional) and the Otolaryngology Resident Talent Assessment (ORTA), a phone-based pre-interview survey to assess personality traits.
“About the time the paragraph was introduced, applications did go down, but it’s hard to know whether the paragraph was really a factor,” said Dr. Schaitkin. “Most program directors didn’t think it had a big impact—most applicants didn’t write a unique paragraph for each residency program.
“We need to change the narrative that an otolaryngology match is unattainable. Mentors should offer students specific information on what they’ll need to match, rather than telling them they just shouldn’t apply to otolaryngology. —David R. Lee, MD
Finding Solutions
Although these concerns are valid, otolaryngology is still a highly sought-after field. “We’re very fortunate that the caliber of the applicants we continue to receive is still excellent,” said Dr. Gray.
“We need to change the narrative that an otolaryngology match is unattainable,” added Dr. Lee. “Mentors should offer students specific information on what they’ll need to match, rather than telling them they just shouldn’t apply to otolaryngology.”
Now in its third year, Ohio State’s student-mentoring program is specifically geared toward first- and second-year medical students. “I think they’re very undifferentiated during those years. With our program, they’re at least aware of our specialty and understand the possibilities of a career in otolaryngology outside of the regular Ohio State curriculum,” said Dr. Elmaraghy.
The four-month program begins with reaching out to first- and second-year students early in the academic year through the school’s otolaryngology interest group and encouraging them to apply, with a stated area of interest (oncology, pediatric, etc.). These students are then “matched” with department mentors. Students are obligated to spend eight to 10 hours per month both in the operating room and clinic, and treated as part of the rotation. A series of lectures cover basic otolaryngology principles and career professionalism topics.
Dr. Gray also believes in the impact of local solutions. “One of our head and neck surgeons, Dan Deschler, MD, partnered with the school to form an interest group for first-year students, working with residents, hosting dinner meetings, and showing videos of what we do. It made a real difference; we’re seeing more sub-interns interested in applying to otolaryngology.”
OPDO, in conjunction with the Academic Deans Association, has crafted a position statement to be sent this year to all medical school deans and advisors. “We want to reach out to make sure that they continue to see otolaryngology as an excellent field for their students to enter,” said Dr. Gray.
Dr. Schaitkin has suggested creating a national medical student otolaryngology curriculum through OPDO to offer to the medical schools, adding that this would increase expertise and heighten awareness of otolaryngology earlier in the education process. “We would come up with a curriculum and then ask every residency program in the country to provide one lecture on one of those topics,” he explained. He’s also requesting institutional review board approval for a survey that would gather data from match participants on their decisions about going—or not going—into otolaryngology.
Even with the downward trend, Dr. Chang remains optimistic. “Ninety-five percent of our spots matched, which is still really good,” he said. “I do think it’s an opportunity for us to soul search a little more about how we present ourselves, and who we look at as suitable candidates.”
Amy E. Hamaker is a freelance medical writer based in California.
Key Points
- ENT has traditionally been a sought-after specialty, but residency applications have dropped in the last two years.
- Experts cite the specialty’s prestigious reputation, additional application requirements, and student desire for more work/life balance among the factors for the decline.