Image Credit: Viktor Gladkov/SHUTTERSTOCK.com
DALLAS—A 37-year-old woman presents with nasal airway obstruction that’s worse on the left, when lying down, and in cold air. Over the past three months, she has tried over-the-counter medications and a steroid nasal spray, with some improvement.
Explore This Issue
November 2015An exam shows that the septum is deviated to the left. Now, questions arise: Do you need to perform a CT scan to document the deviation? How long does she need to try nasal spray before moving on to surgery? What do you need to give the insurer for prior authorization?
These and other questions have been addressed in a new Clinical Consensus Statement on septoplasty from the Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS). The major points of the statement, which offers 20 comments regarding imaging, medical management, and perioperative considerations for septoplasty, were discussed in a session during the annual meeting of the AAO-HNS Foundation, held in Dallas September 27-30.
Performing Nasal Endoscopy with Nasal Obstruction
Scott Stringer, MD, MS, chair of otolaryngology and communicative sciences at the University of Mississippi in Jackson, said he performs nasal endoscopy in cases of a deviated nasal septum approximately three-quarters of the time. “Situations where I would not do it is if the history is crystal clear, [and] there’s nothing unusual whatsoever,” he said.
Timothy Lian, MD, vice chair of otolaryngology at Louisiana State University in Shreveport, said that he performs endoscopy for a deviation approximately 50% to 75% of the time, although he noted that his cases are skewed toward plastic and reconstructive procedures. He added that he would perform nasal endoscopy if he couldn’t explain elements of the history provided by the patient.
The statement also points out that endoscopy could provide “useful information” even when the deviation can be plainly seen. That could help with insurance resistance on coverage of the endoscopy, said Richard Rosenfeld, MD, MPH, senior advisor for guidelines and quality at the AAO-HNS, because physicians can now point to the statement.
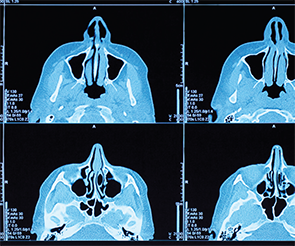
CT to Document a Septal Deviation
If a CT is ordered purely to demonstrate the septal deviation, the vast majority of the statement panel members did not think it was a necessary step, Dr. Stringer said. On the other hand, certain carriers might require the scan in certain cases. Dr. Rosenfeld pointed out that the lack of support for performing a CT scan to establish that a deviation exists was partially due to the drawbacks—it’s costly, it might not be readily accessible, and it involves exposing patients to radiation.
Medical Management with Nasal Sprays before Septoplasty

Image Credit: Creations Naumov/SHUTTERSTOCK.com
The statement says that a trial of medical therapy of more than four weeks is unnecessary to establish candidacy for surgery. In some cases, such as severe caudal septal deviation with complete obstruction, there’s no way that a nasal spray could get into the cavity, Dr. Lian said. In those cases, it seems unreasonable to have a month’s trial of medical management. But, some carriers ask for that. “If there are other elements in the history, such as allergic rhinitis, that are suggestive that they may respond to steroid nasal spray, and if it appears it’s able to be delivered, then a month is a reasonable time,” said Dr. Lian.
Perioperative Antibiotics and Turbinoplasty with Septoplasty
The statement says there is no benefit to administering antibiotics perioperatively unless nasal packing or a splint is placed during the procedure. Dr. Stringer noted that the literature suggests that antibiotics provide no benefit, even in cases with packing or splints, but the experts chose to make an exception in packing or splint cases. “There is a lot of belief in our specialty that splints and nasal packing are different,” said Dr. Stringer. Both he and Dr. Lian added that they very rarely use packing or splints anyway.
Dr. Stringer also advised that, even though insurers sometimes are hesitant to approve coverage for turbinoplasty in addition to septoplasty, the panelists “came to a consensus fairly rapidly” that the turbinates need to be addressed as well. “I think it’s important that we have that in there,” he said. “We’re not really treating the septum alone. We’re treating an airflow issue.”
Septoplasty and OSA
The statement says that septoplasty can improve continuous positive airway pressure (CPAP) tolerance for patients with obstructive sleep apnea (OSA) and a deviated septum, but does not say that septoplasty alone directly improves OSA.
The panel also emphasized the improved sensation of nasal airflow. “The perception is that when a patient lies down to sleep that they can then breathe unobstructed through their nose,” he said. “While it may not change their polysomnography, the patient’s happiness is improved.”
Thomas Collins is a freelance medical writer based in Florida.
Take-Home Points
- Nasal endoscopy can provide useful information prior to septoplasty, such as other causes of nasal obstruction, even when anterior rhinoscopy documents septal deviation.
- A CT scan of the paranasal sinuses is unnecessary to document the septal deviation prior to septoplasty but may be useful in diagnosing other sinonasal pathology in patients with symptoms that cannot be explained by septal deviation.
- A trial of medical therapy for more than four weeks is unnecessary to assess surgical candidacy for septoplasty.
- There is no benefit to routine peri-operative antibiotics during septoplasty unless nasal packing or a splint is placed during the procedure.
Consensus Statement vs. Guidelines
As defined by the Institute of Medicine, consensus statements are different from guidelines in that they’re essentially opinions on topics that are considered important and controversial but for which there is not enough high-level evidence for a clinical practice guideline. “There are a lot of questions that come up that we grapple with as clinicians, and there aren’t any randomized trials to help us out,” said Richard Rosenfeld, MD, MPH, senior advisor for guidelines and quality at the AAO-HNS. “The purpose of this [statement] was to get a meeting of the minds and, using a fairly systematic rigorous process, to try to identify important areas of consensus that could reduce uncertainty and improve the quality of patient care.”
Consensus statements come from a group of experts who are well versed in the evidence and the condition, while guidelines do not necessarily come just from experts, but from panels that include experts, consumers, or other physicians—each representing a specific stakeholder perspective.
The statements are developed using the Delphi method: A statement is made, and each of the panelists rates his or her level of agreement on a 0 (strongly disagree) to 9 (strongly agree) scale. If the average is at least 7, without significant outlier responses, the statement is accepted. If there is no consensus, it is dropped. If it falls in the middle, the panelists discuss it and then re-assess the statement.
“If you can reach a good consensus on it, then that’s something worth knowing, and something you may want to do in your practice,” Dr. Rosenfeld said. “But we’re not making a recommendation.”—TC