Presentation: A 64-year-old female presented to the emergency department complaining of shortness of breath. This patient stated that she has had some progressive dyspnea and dysphagia for approximately six months. Physical examination revealed an afebrile female with tachypneic respirations and no stridor. Flexible fiberoptic exam revealed an obstructive submucosal process emanating from the retropharynx extending to the level of the epiglottis and obscuring the endolarynx.
The patient was quickly brought to the operating suite where flexible fiberoptic intubation was attempted, but visualization was obstructed secondary to the mass. A tracheotomy was then performed after the patient underwent rapid respiratory decompensation.
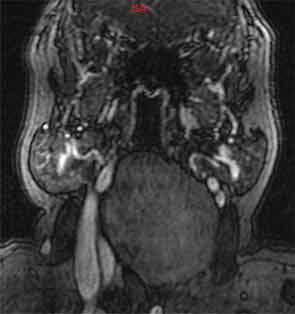
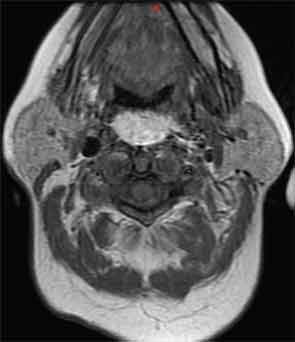
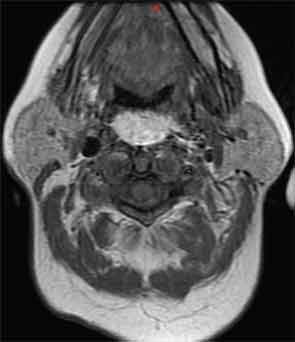
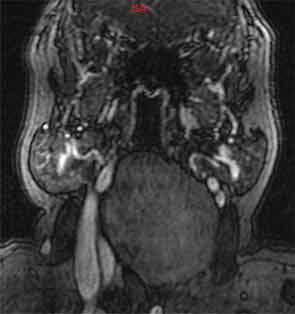
Axial and sagittal contrast enhanced computed tomography of the neck (Figure 1a, 1b) showed a 8.3 x 4.4 x 8-cm low-density retropharyngeal mass. Axial MRI T1 images (Figure 2) exhibited high signal intensity, while coronal T2-weighted images (Figure 3) revealed low signal intensity.
—John Carter, MD; Ryan Chastant, MD; Paul Friedlander, MD; Rizwan Aslam, DO, Tulane University School of Medicine, New Orleans.
What is your diagnosis, and how would you manage this patient? Go to the next page for the answer.
Management
CT-guided fine-needle aspiration (FNA) of the mass was performed. Preliminary evaluation by the cytopathologist revealed multiple fat globules on the slide, which dissolved with alcohol, establishing the lipomatous nature of the lesion. The patient underwent transcervical excision, yielding an 8.0 x 7.0 x 2.5-cm yellow-tan glistening mass that was consistent with lipoma. One month after tumor removal, the patient was swallowing well, had no airway issues and was able to be successfully decannulated.
Discussion
Lipomas are benign, slow-growing neoplasms of mesenchymal origin that may appear in the retropharyngeal space. The retropharyngeal space is defined as the space posterior to the pharyngeal mucosa and anterior to the prevertebral fascia. Primary tumors of this location are rare. The retropharyngeal space contains lymph nodes, along with a small amount of fat from which these lesions are thought to stem. Retropharyngeal lipomas most often originate from the infrahyoid retropharyngeal space.1
The clinical course can be insidious. Subtle dysphagia, shortness of breath and obstructive sleep apnea have been described as presenting signs. Symptoms may be present for months to years and increase at a slow pace. Furthermore, the retropharyngeal and parapharyngeal spaces provide a large area in which a tumor can spread without the patient noticing. As in this case, the patient may not seek medical treatment before experiencing acute airway obstruction.
The radiographic characteristics of retropharyngeal lipomas are typical of lipomas in other anatomic locations. They appear as homogenous low attenuation masses with no clearly defined capsules that resemble fat, with -50 to -150 Hounsefield units.2,3 Heterogeneity on CT may indicate a liposarcoma, while an irregular interface may suggest an infiltrating lipoma. MRI, will reveal a hyperintense lesion on T1 that does not enhance with gadolinium. MRI may be useful in the identification of a liposarcoma: Thickened septa, associated non-adipose masses, prominent foci of high T2 signal and prominent areas of enhancement are associated with this entity.4
Histologic diagnosis, in some circumstances, may be necessary to differentiate lipoma from liposarcoma. Complex capillary networks, increased cellularity, lipoblasts, and metachromatic stroma are present in liposarcoma and can alert the practitioner to a mass that needs to be removed urgently. Fat cells may be all that is yielded on FNA and cannot be differentiated from normal fat until final removal of the lesion.5
Treatment is surgical excision and is accomplished through an intraoral or transcervical approach, depending on the extent of the lipoma. Pre-operatively, if an infiltrating lipoma is suspected, wide local excision (WLE) including a cuff of pre-vertebral musculature should be undertaken. The rate of recurrence of an infiltrating lipoma, without WLE, is as high as 62.5 percent.5,6
Conclusion
In the case of acute airway compromise, the obstructing lesion may be quite large, possibly complicating the ease of obtaining a secure airway. Awake flexible fiberoptic intubation may be attempted initially; however, the practitioner should be prepared for emergent tracheostomy if the airway cannot be secured through intubation. The operating room is the safest environment to manage this potentially challenging situation.
References
- Senchenkov A, Werning JW, Staren ED. Radiographic assessment of the retropharyngeal lipoma. Otolaryngol Head Neck Surg. 2001;125:658-660.
- Aland JW Jr. Retropharyngeal lipoma causing symptoms of obstructive sleep apnea. Otolaryngol Head Neck Surgery. 1996;114:628-630.
- El Fortia M, El Fagieh M, Khalil M, Elhamroush H, Eldergash O, El Gatit A. A massive retropharyngeal lipoma. European Journal of Radiology Extra. 2006;57:9-12.
- Gaskin CM, Helms CA, Lipomas, lipoma variants, and well-differentiated liposarcomas (atypical lipomas): results of MRI evaluations of 126 consecutive fatty masses. Am J Roentgenol. 2004;182:733-739.
- Hockstein NG, Anderson TA, Moonis G, Gustafson KS, Mirza N. Retropharyngeal lipoma causing obstructive sleep apnea: case report including five-year follow-up. Laryngoscope. 2002;112:1603-1605.
- Dionne GP, Seemayer TA. Infiltrating lipomas and angiolipomas revisited. Cancer. 1974;33:732-738.
Leave a Reply