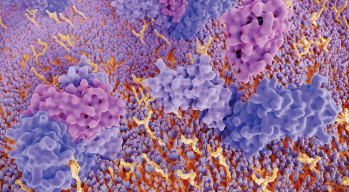
Interleukin 4 (IL-4) binds to its receptor.
© Juan Gaertner / shutterstock.com
The possibility of utilizing biologic therapies for chronic rhinosinusitis (CRS), an inflammatory condition of the sinonasal mucosa, is a growing area of interest and research. This rise in interest is due in part to the success of biologics in treating other inflammatory conditions such as asthma and atopic dermatitis. A panel of experts gathered at the Triological Society Annual Meeting discussed the biologics that are being explored for CRS and nasal polyposis.
Explore This Issue
June 2019Jean Kim, MD, PhD, an associate professor of otolaryngology–head and neck surgery at Johns Hopkins University School of Medicine in Baltimore and panel moderator, said, “What makes antibodies so attractive is the specificity for the target. However, there are some previously reported uncommon nonspecific effects that may be detrimental, such as immunosuppression, cardiomyopathy, new cancer, and cytokine storm. Additionally, autoantibodies and allergy to the antibodies have also been reported.”
What is known about the biology of nasal polyps (NP) comes from understanding similarities with asthma, he said. In fact, he added, the rationale for NP drug development originates from studies of severe asthma. Both display similar patterns of Th2 (or type 2) inflammation. Their behavior is also similar, with both displaying a responsiveness to steroids. Thus, the targets that mediate Th2 inflammation are the biologic drug targets that are being developed for nasal polyposis, which include IgE, IL5, IL4, and IL13.
Dupilumab
Joseph K. Han, MD, director of the division of rhinology and endoscopic sinus and skull base surgery and medical director of the division of allergy at Eastern Virginia Medical School in Norfolk, and his colleagues recently completed a phase 3 trial on the use of dupilumab, which blocks IL-4 and IL-13, for nasal polyposis. This medication received priority review by the FDA, and full approval would make it the first biologic approved by the FDA to treat CRS with NP (CRSwNP), he said.
His study, which involved 276 patients, concluded that dupilumab is safe and effective for CRSwNP. Patients treated with this drug showed progress in as early as four weeks and experienced a reduction in the size of polyps, the severity of nasal congestion, and the need for surgery or steroids, said Dr. Han. These improvements continued through week 24, and the need for surgery in these patients was reduced by 73%.
The two primary outcomes, nasal congestion and NP, were both statistically significant, he added. Regarding congestion specifically, those who had medium to severe congestion at the outset of the study had zero to mild congestion by the end of the study.