Basic science departments serve three key missions: to conduct research, to teach graduate students in basic science fields, and to teach medical students. But basic science departments at academic institutions are hurting. They face challenges such as insufficient funding, dwindling faculty numbers, shrinking curriculum, and limited research space. Ultimately, these challenges negatively impact the medical field in a variety of ways.
Explore This Issue
July 2019Funding Issues
Basic science departments are predominantly funded by grants to support research. Typically, these departments don’t have a means to create revenue on their own, as clinical departments do through compensation for clinical work. “While there may be some state funding for specific investigators, these salary lines are few and far between and certainly aren’t enough to support a complete and modern department,” said Andrew Murr, MD, professor and chair of the department of otolaryngology–head and neck surgery at the University of California, San Francisco. “Endowed positions sometimes exist to help with support, but basic science departments have little interaction with the public, so raising money through philanthropy is less likely,” he added.
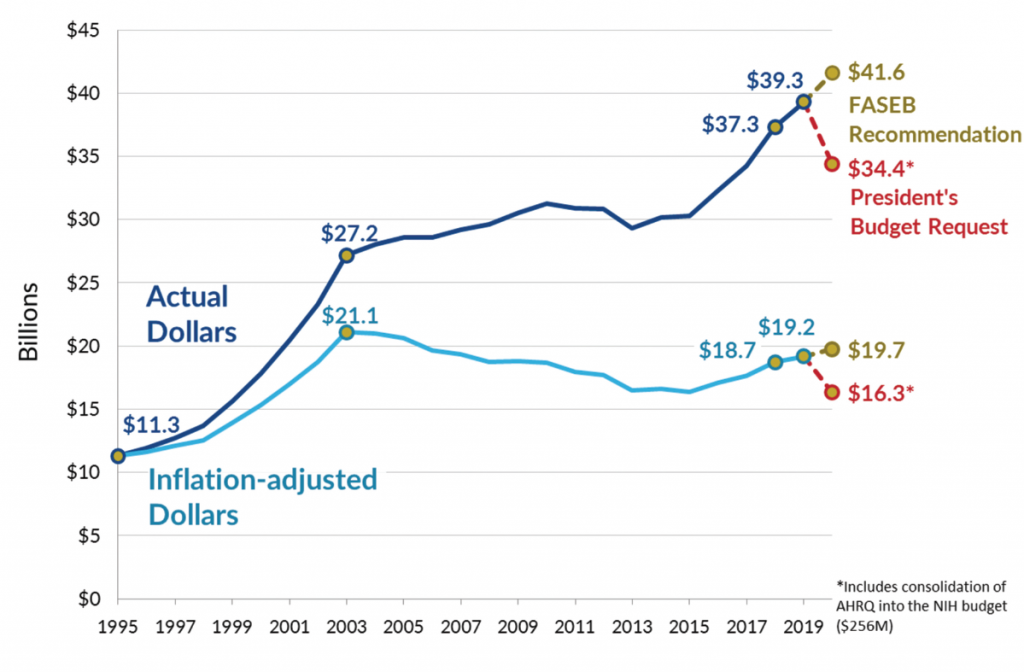
Although there have been significant improvements in the federal government’s budget for the National Institutes of Health (NIH) in recent years, when adjusted for inflation, the budget is still smaller than it was in 2003. “Basic scientists have experienced 15 years with no growth in available resources, with terrible pay lines from NIH and National Science Foundation grants,” said Ross McKinney, MD, chief scientific officer of the Association of American Medical Colleges (AAMC).
Wendell G. Yarbrough, MD, MMHC, a professor and chair of otolaryngology/head and neck surgery at the University of North Carolina at Chapel Hill, had similar sentiments. “Many NIH institutes are funding applications in the single-digit percentiles, and when grants are funded they oftentimes aren’t large enough for the proposed research to be completed,” he said. In addition, salary caps on NIH grants create another funding gap. Funding from clinical sources or schools of medicine are also under pressure due to decreased reimbursement for clinical activity, so making up for lost funding is particularly challenging.
Dr. Murr added that with funding becoming increasingly tight for NIH awards, the funding line is becoming more exclusive, so fewer young scientists can get comfortably and firmly established. Furthermore, “if a researcher has an extremely compelling grant but their institution’s environment isn’t devoted to their topic of interest, they may be left out of funding,” he said.
The erosion of academic pursuits in schools of medicine risks the leadership roles that schools have held and will ultimately slow innovation that would benefit patients. —Wendell G. Yarbrough, MD, MMHC
Dwindling Faculty Numbers
Developing and maintaining fruitful collaborations among clinical and basic science researchers is critical to a strong research program—especially collaborations that lead to translational and clinical research that directly benefits patient outcomes, said Judy R. Dubno, PhD, director of research in the department of otolaryngology–head and neck surgery at the Medical University of South Carolina in Charleston. But both basic science and clinical researchers face challenges in dedicating effort to collaborations and translational research, given the pressure to maintain their individual research programs with funding and their clinical practices.
A thriving research program also requires a strong infrastructure, including administrative personnel to assist with grant management, continually growing and changing policy and regulatory requirements, and other essential administrative tasks essential for conducting research, all of which add to overhead costs, Dr. Dubno said.
Finally, there is an urgent need for basic science faculty, departments, and medical schools to support the unique requirements of physician–scientists, Dr. Dubno added. To ensure the continued growth of the science that underlies otolaryngology health and disease, basic science faculty in otolaryngology–head and neck surgery departments must fully participate in an enriched educational and scientific environment that values research and research training as high priorities.
Given the limited funding that medical schools receive and the low rates of grant awards, bridge funding, a form of temporary and immediate funding for investigators whose grants have lapsed, is becoming more commonplace. Consequently, faculty members may not be able to continue their research if bridge funding is not available, Dr. Yarbrough said.
Limited funding for research has resulted in little or no growth in the number of faculty in basic science departments. AAMC data show that there were roughly the same 20,000 faculty in basic science departments in toto across the United States over the last decade. In 2009, there were 18,526 basic science faculty, and in 2018 there were 19,732—a 7% increase. However, at the same time there was a 21% increase in the number of medical schools.
A related challenge stems from the fact that the median age for a medical school faculty member as of 2015 was around 50. Although staffing shortages aren’t a current problem, aging faculty are holding positions that could be filled by more recent graduates, but those slots aren’t available due to caps on the number of tenure-track salary lines.
Furthermore, Dr. Murr pointed out that losing scientists to industry is commonplace. “The biopharmaceutical industry can often pick off successful professors who are well established or successful post docs who are daunted by the extraordinary costs and pressures to set up a laboratory,” he added.
Shrinking Curriculum
Historically, basic scientists taught medical students in the first two years of the medical school curriculum. The standard model was that a faculty member would give a few lectures and perhaps run a course in their area of expertise. Students learned information through lecturing, but most schools are now moving to models that involve team-based learning or a problems-based curriculum, and some schools have completely eliminated lectures. As a result, the medical student teaching justification for basic science faculty has diminished substantially, and some schools are shifting dollars from basic science departments to the medical student teaching program.
Dr. McKinney added that teaching graduate students in the basic sciences continues to be an important role for basic science departments, a function supported by tuition dollars and by grants. However, attrition of faculty at some graduate schools means that programs are losing the critical mass of faculty necessary to sustain a basic science graduate program.
The lack of stable, long-term funding also makes it difficult to build and expand new programs and recruit and retain basic science faculty, Dr. Dubno said.
On the positive side, doctoral degree graduates in the biomedical sciences are very employable, Dr. McKinney said. The majority of them go into jobs that aren’t within academia, but rather in industry, government, or research.
Space Limitations
Departments also struggle with limited availability of high-quality space for clinical and basic science laboratories, Dr. Dubno said. Additionally, available space is rarely co-located with space designated for clinical faculty or basic science faculty who work in different sub-disciplines, which reduces opportunities for effective collaborations among clinicians and basic science faculty. Similarly, equipment, up-to-date technologies, and necessary renovations may be lacking due to limited intramural or extramural funding.
The Greater Impact
The balance among clinical care, education, and research is being tilted toward clinical care—which is the major source of income for a school and its affiliated hospitals. This results in a lower emphasis on and fewer funds invested in the basic sciences. “The intermediate to long-term risk is that academic basic science departments become more marginalized with fewer investigators,” Dr. Yarbrough said. “The erosion of academic pursuits in schools of medicine risks the leadership roles that schools have held and will ultimately slow innovation that would benefit patients.”
Dr. McKinney said that huge opportunities to improve care in hearing restoration and communications disorders will require more knowledge of how the brain processes acoustic signals at everything from the cellular level to the neuronal networks that respond and interpret the information. “But if basic science departments suffer, progress will be limited,” he said.
Because they have close relationships with basic science departments through collaborative research, shared faculty, and curricula that emphasize the intersection of basic and clinical knowledge, otolaryngology departments will face challenges for maintaining academic and educational missions. “Diminution of basic departments will make these challenges more acute,” Dr. Yarbrough said. “Strong basic science departments within medical schools are needed to train the next generation of otolaryngologists and to partner with otolaryngology faculty to advance our understanding and treatment of diseases of the upper aerodigestive tract.”
Karen Appold is a freelance medical writer based in New Jersey.
Key Points
- The balance among clinical care, education, and research is tilting toward clinical care.
- Limited funding for research has resulted in little or no growth in the number of faculty in basic science departments.
- The lack of long-term funding makes it difficult to build new programs.
Six Ways to Help Basic Science Departments Regain Vitality
Keeping basic science departments running optimally is a growing challenge, but experts say some things can be done to help them regain their strength. Here are six suggestions.
- Support funding for the NIH. “There have been meaningful, greater-than-the-rate-of-inflation increases in the NIH budget each year since 2015,” Dr. McKinney said. “That has helped to heal the damage done by years of inadequate funding.” But schools of medicine will need to continue to support basic science financially, because NIH grants have never paid the full cost of basic science research. NIH funding is critical for basic science, and without it there won’t be the types of new ideas necessary for translation into novel clinical applications.
- Form partnerships. Basic science departments can partner with industry and clinical departments to increase research portfolios that are closer to clinical implementation, which could open new funding sources, said Dr. Yarbrough. In addition, academic hospitals and centers within medical schools should continue to invest wisely in basic science departments.
- Promote effective communication. Teach students to communicate their research to others in a clear, concise way. “We need the public (taxpayers) to understand what basic scientists do,” Dr. McKinney said. “Their support is necessary to sustain the basic science culture.”
- Ask public relations offices to avoid hyped language. “Hype can ultimately hurt basic science departments,” Dr. McKinney said. “The public will lose trust in science if they’re constantly being bombarded with false claims like there’s a new cure for cancer. When taxpayers lose their faith, funding will dry up.”
- Train doctors of philosophy to be flexible. “Don’t just train doctors of philosophy to be the next generation of faculty, train them to be the next generation of researchers for whatever environment they may find themselves, such as academia, industry, or government,” Dr. McKinney said.
- Help develop better pathways for junior investigators. “We need to make it easier to have a good career in basic science,” Dr. McKinney added. “This means that schools need to provide adequate resources to financially support junior faculty until they’re able to get federal grant funding.”