
Six years after balloon sinuplasty was introduced to the otolaryngology community, it remains an evolving technology. “In my opinion, balloon dilatation has great potential, but it’s still trying to find its proper place in the ENT arena,” said Ralph Metson, MD, clinical professor of otology and laryngology at Harvard Medical School and Massachusetts Eye and Ear Infirmary in Boston.
Balloon sinuplasty, sometimes also called balloon catheter dilatation, was originally envisioned as a less invasive alternative to endoscopic sinus surgery for patients who had failed to find relief with medical management of chronic rhinosinusitis. Few studies, though, have compared the two procedures. A recent Cochrane review found just one unpublished study that randomized 34 patients to either balloon dilatation or functional endoscopic sinus surgery (FESS). The review authors concluded that “at present, there is no convincing evidence supporting the use of endoscopic balloon sinus ostial dilation compared to conventional surgical modalities” (Cochrane Database Syst Rev. 2011;6(7):CD00851).
Otolaryngologists around the country, however, are finding balloon sinuplasty to be a useful adjunct to FESS. The procedure also appears to have found a role in the treatment of chronic rhinosinusitis in children.
Functions and Limitations
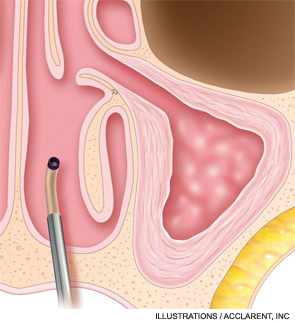
Multiple studies have proven the safety of the technique, which was approved by the U.S. Food and Drug Administration in 2005 (Ann Otol Rhinol Laryngol. 2006;115:293-299; Otolaryngol Head Neck Surg. 2007;137:10-20; Am J Rhinol. 2008;22:204-209). Short-term follow-up has demonstrated good results as well. Recent uncontrolled retrospective and prospective studies have shown sinus patency and improved quality of life scores up to two years after balloon sinuplasty (Postgrad Med. 2011;123(2):112-118). Long-term efficacy is not available because the technique is still rather new.
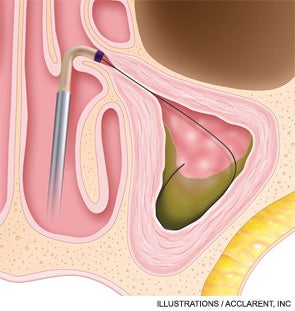
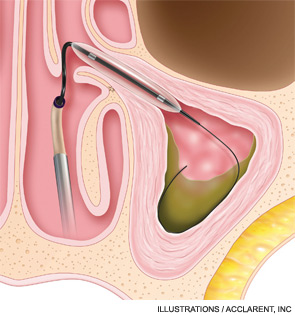
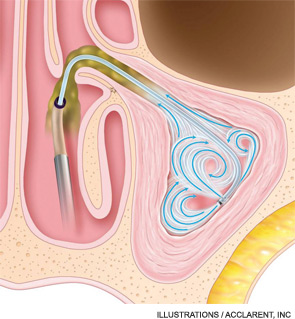
To date, balloon sinuplasty seems to be most useful for dilating the frontal sinus ostia. “Many surgeons are using balloon technology as their main way to enter the frontal sinus,” said Michael Setzen, MD, president of the American Rhinologic Society. “The nasofrontal recess sometimes can be quite difficult to find and to enlarge. When we use a wire with a light on the end, we know we’re in the sinus and then we can pass our balloon over that wire and dilate the nasofrontal sinus.”
Balloon catheter technology is also approved for use in the maxillary and sphenoid sinuses; it is not for use in the ethmoid sinus. “If a patient has ethmoid disease, you’re going to have to use some other tools to treat that,” said Kevin McLaughlin, MD, assistant clinical professor of rhinology, sleep medicine and sinus surgery at Louisiana State University Health Sciences Center in New Orleans.
A Cure—or an Adjunct?
Despite the early hype suggesting that balloon sinuplasty might be an alternative to sinus surgery for some patients, most otolaryngologists are use the balloon in conjunction with functional endoscopic sinus surgery.
“I perceive the balloon as a tool that we have at our disposal to treat the sinuses,” said Dr. McLaughlin, who often combines balloon sinuplasty with FESS. Dr. Setzen also performs hybrid procedures.
“There are times when one may just want to dilate one sinus, say a frontal sinus, but yet do traditional work on, say, the other frontal and/or maxillary sinus,” Dr. Setzen said. “You may also use the technology to enter a sinus and then utilize traditional surgery to further enlarge the opening of that sinus once the technology has helped you find the opening.”
David Kennedy, MD, professor of rhinology at the University of Pennsylvania School of Medicine in Philadelphia and an early innovator in the field of sinus surgery for chronic rhinosinusitis, is concerned that balloon sinuplasty may not address the underlying issues of sinusitis and, therefore, may not lead to the cure that many patients expect.
“Resolving chronic sinusitis is not just a matter of drainage,” Dr. Kennedy said. “If it was a simple plumbing problem, we wouldn’t have so much chronic sinusitis around. Just opening up the sinus is rarely a solution to resolving well-established surgical disease.”
Dr. Kennedy and others now believe that inflammation of the bone contributes to chronic sinusitis, and hypothesize that just moving the bone aside with a balloon may lead to continued difficulty. Therefore, Dr. Kennedy suggests removing the bone fragments, although no studies have tested the efficacy of this approach.
“The balloon provides a very easy and relatively atraumatic way of fracturing the bony partitions in the sinuses,” Dr. Kennedy said. “We use the balloon as a tool to open up the sinus ostium, then we tease out the bony partitions once they have been fractured.”
Pediatric Patients
Balloon sinuplasty is increasingly used in the pediatric population. Hassan Ramadan, MD, professor of otolaryngology at West Virginia University in Morgantown, was one of the first to demonstrate the safety and efficacy of the procedure in children (Ann Otol Rhino Laryngol. 2009;118(3):161-165; Amer J Rhino Allergy. 2010;24(1):e54-56).
“Most people are a little hesitant to go in and perform an endoscopic sinus surgery procedure on kids,” Dr. Ramadan said. “They think it’s maybe a little bit too aggressive, that these kids eventually will outgrow the problem, as their immune system gets better. So, this seemed to me like the perfect fit. Instead of going and doing an endoscopic sinus surgery, you use the balloon, because using the balloon, you’re not taking any tissue out. You’re not disrupting the anatomy.”
Balloon sinuplasty may improve the post-surgical care of children who undergo sinus surgery. “In the past, with traditional sinus surgery, we’d have to potentially take them back to the operating room so that we could perform postoperative endoscopy and any manipulation to the wound that was necessary,” Dr. McLaughlin said. “I started using the balloon with children because I saw it as an opportunity to treat a child’s sinuses and not have to take them back to the operating room for postoperative debridement.”
According to Drs. Ramadan and McLaughlin, the use of balloon sinuplasty does not rule out the use of FESS at a later date, should it become necessary.
New research suggests that combining balloon sinuplasty with adenoidectomy, a traditional treatment for chronic rhinosinusitis in children, may improve outcomes. While adenoidectomy typically provides relief to about 50 percent of children who undergo the procedure, a 2010 study by Dr. Ramadan found that 80 percent of children treated with balloon sinuplasty and adenoidectomy experienced an improvement in symptoms (Ann Otol Rhino Laryngol. 2010;119(9):578-582). The improvement persisted 12 months after surgery: 80 percent of children who received the combined treatment experienced significant improvement, compared with 52.6 percent in the group that had undergone adenoidectomy alone.
Appropriate for the Office?
While some physicians are using balloon sinuplasty in conjunction with traditional surgical techniques in the operating room, others are eyeing the technology for use in the office.
“There’s definitely a move towards office-based procedures,” Dr. Setzen said. However, proper patient selection will be essential if office-based balloon sinuplasty is to take off, and research studies that identify proper patient populations are lacking. “I don’t really know exactly who are the best patients for the balloon technology,” Dr. Metson said. “The proper patients and the proper disease are still somewhat unclear.”
Dr. Setzen suggests that all candidates for sinus surgery, whether for balloon sinuplasty or FESS, meet the following criteria:
- Documented history of sinusitis;
- Endoscopic exam of the sinuses, demonstrating blockage; and
- History of maximum medical therapy.
Patients with a markedly deviated septum or advanced sinus disease are not candidates for in-office balloon sinuplasty. Neither are children, because children lack the ability to sit still while the surgeon manipulates tools in their sinuses. “I do simpler cases in the office, patients who may have just one or two blocked sinuses without a badly deviated septum and no polyps,” Dr. Setzen said. “If there’s significant sinus disease, I wouldn’t want to do it in an office setting.”
In-office balloon sinuplasty may be attractive for some patients and physicians, but Dr. Setzen said that physicians considering the procedure must make sure they’re adequately equipped. “You need more office personnel to assist you if you perform balloon dilatation in office. You may need an assistant, a circulator in the room and additional technology. You also need to have appropriate monitoring and life support. These are all additional risks for the physician and an added liability.” “The good news is that the potential risks following the operation are pretty low,” said Dr. Setzen. Reported complications of balloon sinuplasty include turbinate lateralization or scarring (Am J Rhinol. 2008;22:204-209). To date, no research studies have examined the safety or efficacy of in-office balloon sinuplasty.
Patient Demand
Some physicians believe that direct-to-patient marketing is fueling the demand for balloon sinuplasty.
“The economic push with balloon sinuplasty is really greater than any I’ve seen,” Dr. Metson said. “Many of us, the first time we ever heard about balloons was in press releases rather than the medical literature. Our patients were asking us to do it, before any studies were out whatsoever.” The physicians who were interviewed for this article emphasized the importance of establishing realistic expectations. Some patients, based on advertising, come to the physician expecting a minimally invasive, in-office procedure that will cure their chronic rhinosinusitis. The reality, as Dr. Kennedy and others have stated, is often more complicated, and many patients will need traditional sinus surgery in addition to balloon sinuplasty.
That reality has caused some of the initial excitement regarding balloon sinuplasty to wane among physicians.
“At this point in time, a lot of the initial enthusiasm for a strictly balloon approach has dropped off,” Dr. Kennedy said. “Any time a new technology is introduced, there’s this pendulum swing where everyone gets very excited about it and then people become disillusioned and then the technology eventually finds its accurate position. With balloon sinuplasty, we’re just starting to find out what its real position may be.”
Added Expense
Because balloon sinuplasty requires disposable equipment, its cost is typically higher than that of FESS. That additional cost is causing some physicians and hospitals to rethink their use of the procedure.
“The cost of the disposables for doing balloon dilatation is often over $1,000 per case,” Dr. Metson said. “Let’s say you have a hospital whose profit margin might be $1,000 or less per case. That can take a profitable procedure and make it a nonprofitable one for a hospital. Because of that, I know many of my fellow physicians are getting heavy pressure from their hospitals to reduce the number of balloon sinuplasty cases.”
Dr. Metson believes that the procedure’s high costs, coupled with potentially higher reimbursement rates for out-of-hospital procedures, is at least partly behind the drive toward in-office balloon sinuplasty.
The Future
One thing seems clear: Balloon technology will continue to be part of sinus surgery in the foreseeable future. Patient demand, coupled with clinical investigations into additional uses of the technology, will make balloon dilatation a must-have skill for most sinus surgeons.
“This is a very significant new technology that’s being used in the management of sinus disease,” Dr. Setzen said. “I would say that anybody doing endoscopic sinus surgery today needs to be at least trained and aware and knowledgeable about the use of the balloon.”
Leave a Reply