 Balloon dilation originated in cardiac catheterization procedures and has become reasonably common in otolaryngology, most notably as balloon sinuplasty. Eustachian tube balloon dilation, however, is a more recent variant of the procedure that was approved for adults by the Food and Drug Administration (FDA) in 2016 and is currently performed only off label in children in the United States.
Balloon dilation originated in cardiac catheterization procedures and has become reasonably common in otolaryngology, most notably as balloon sinuplasty. Eustachian tube balloon dilation, however, is a more recent variant of the procedure that was approved for adults by the Food and Drug Administration (FDA) in 2016 and is currently performed only off label in children in the United States.
Explore This Issue
April 2023But to his surprise, it did.
“The lesson learned is that you have to keep an open mind, because it actually was working much better than we thought it should,” he said. “We observed in our patients that it really was quite remarkable in reducing inflammation.”
I basically tell people we stumbled on this technology that turns out to be very effective for doing an adenoidectomy in a narrow tube that we previously couldn’t access. —Dennis Poe, MD, PhD
Although they didn’t understand the mechanism by which the balloon was working at first, they later performed biopsies and discovered that the balloon was crushing the inflamed mucous membrane and adenoid-like tissue in the submucosa; it was essentially like performing an adenoidectomy on the tissue clogging the Eustachian tube.
“I basically tell people we stumbled on this technology that turns out to be very effective for doing an adenoidectomy in a narrow tube that we previously couldn’t access,” he said.
Before Dr. Poe and his colleagues published their findings in 2011, German otolaryngologist Thorsten Ockermann, MD, and his colleagues published a study on cadavers that concluded that BDET seemed to be a feasible and safe procedure to dilate the Eustachian tube (Otol Neurotol. 2010;31:1100–1103). Dr. Poe was one of many people who helped design the first FDA approved device in the United States. He said that a series of recent meta analyses and reviews have shown very favorable results.
In 2019, the American Academy of Otolaryngology–Head and Neck Surgery (AAO-HNS) released a set of clinical statements on BDET use (Otolaryngol Head Neck Surg. 2019;161:6–17); Dr. Poe and rhinologist Edward McCoul, MD, MPH, a professor and vice chair in the department of otolaryngology at Ochsner Medical Center in New Orleans, were among the co-authors. “The most relevant takeaways were related to the diagnosis and identification of Eustachian tube dysfunction,” Dr. McCoul said, “which remains to be fully standardized.”
Some of the areas of consensus in the statements were that audiometry, specifically tympanometry, is required in the assessment. Nasal endoscopy is also strongly encouraged, as well as functional assessment, such as the ability to perform the Valsalva maneuver. All of these, Dr. McCoul said, should be abnormal in obstructive Eustachian tube dysfunction.
“This needs to be distinguished from other types of Eustachian tube dysfunction such as patulous dysfunction, or non-obstructive Eustachian tube inflammation,” he said, adding that as far as the current evidence shows, it’s only patients with obstructive Eustachian tube dysfunction who really benefit from balloon dilation of the Eustachian tube.
BDET in Clinical Practice
Steven D. Pletcher, MD, residency program director at the University of California, San Francisco and a head and neck surgeon who specializes in sinus surgery and rhinology, said he currently uses BDET in his practice several times a year. An expert in minimally invasive endoscopic procedures of the paranasal sinuses and skull base, Dr. Pletcher’s practice focuses more on sinus disorders, but he has had patients with comorbid sinus and Eustachian tube disease.
“Sometimes my otology colleagues ask for help with this transnasal procedure due to nasal or sinus disorders that limit access to the Eustachian tube orifice,” he said. “It’s helpful to have an option other than medical management and tympanostomy tubes for these patients, though it’s still hard to know what long-term outcomes will look like.”
James E. Saunders, MD, an associate professor of otology and neurotology at Dartmouth Hitchcock Medical Center in Lebanon, N.H., has been performing the procedure since 2014 and does about one per week, with most of those for patients undergoing middle ear surgery, such as laser myringoplasty or tympanoplasty.
“Patients undergoing BDET are often treated by comprehensive otolaryngologists as an alternative to tympanostomy tubes,” he said. “But I’m interested in determining if this technique can be appropriately used for patients with more severe ear disease.”
Traditionally, Dr. Saunders, who learned this procedure from Dr. Poe, would treat Eustachian tube dysfunction in those patients with tympanostomy tubes, but as these can further weaken the eardrum and lead to perforations, he’s looking for any opportunity to improve function and outcomes. “As an otologist, we’re often at the mercy of the Eustachian tube,” he said.
Dr. Saunders has noticed BDET’s rapidly growing popularity, which he said is often the case when something is fairly easy to perform and carries a relatively low risk. He is concerned, however, that as a specialty, otolaryngologists should be careful about critically evaluating their results and identifying which patients are most likely to benefit.
“We should examine the nasopharynx and Eustachian tube more often when considering middle ear surgery to identify any treatable pathology or potential benefit from BDET,” he said. “We also need to resolve the role of BDET in children and clarify the required pre-op evaluation.”
While there have been a few randomized controlled trials demonstrating the effectiveness of BDET for patients with relatively mild Eustachian tube dysfunction, according to Dr. Saunders, there has been very little research on chronic ear disease.
Dr. Poe noted that it’s difficult to judge how common BDET is in the United States because healthcare providers here don’t keep track of the numbers of these procedures being done.
Performing BDET requires special certification, either from taking a course from the company that sells their balloon device or through training in residency. “There are three FDA-approved devices in the United States, made by Acclarent, Stryker, and Medtronic,” Dr. Poe said. “If you’ve already used the Stryker device for sinuses, you don’t have to get certified for Eustachian tubes. At the academy course, about 70% say they have done the procedure. It’s become a widespread clinical treatment.”
While BDET isn’t yet FDA approved for use in children, Dr. Poe said it’s very popular in other countries and performed on children as young as 18 months. “The balloons we have in the United States aren’t designed for children,” he said. “There’s only one size.”
Dr. Poe has published research on BDET in children aged seven and said that children are very sensitive and there’s risk of overdilation where the valve won’t close, so it’s important to be especially careful in selecting patients. He’s comfortable performing it in children aged five and above, scaling down the amount of time that the balloon is used, but says smaller balloons and more research are needed.
Balloon Dilation-Assisted Cricoid Split Procedure
Balloon dilation has also been used in rib graft placement via an endoscopic posterior cricoid split, a novel modification described by Ahmed AlAmmar, MD, at King Saud University in Riyadh, Saudi Arabia, senior author of a study published last January in The Laryngoscope with co-author and colleague Bshair Aldriweesh, MD, associate consultant, pediatric otolaryngology and airway surgery, King Fahad Specialist Hospital Dammam, Dammam, Saudi Arabia (Laryngoscope. 2022;132:212–214).
According to the study, endoscopic posterior cricoid split and rib grafting (EPCS/RG) was performed in patients with subglottic stenosis, posterior glottic stenosis, and bilateral vocal fold paralysis. Placement of the cartilage graft into the divided cricoid lamina is considered a challenging step in this procedure and the study presents a modified EPCS/RG that used balloon dilation between October 2017 and April 2021 with five patients, ages 11 to 19, to aid in this step. The main outcome measures were resolution of dyspnea, prevention of aspiration, and the need for more surgeries.
Dr. Aldriweesh, who also uses balloon dilation for Eustachian tube dysfunction and subglottic and/or tracheal stenosis, said she liked using balloon dilation in this case for providing a means to expand a stenotic area with a high-pressure mechanism, facilitating a graft insertion into the cricoid split.
According to the study, compared to the traditional transcervical approach, EPCS/RG has a reduced operative time and aspiration risk, is associated with minimal morbidity, and does not require a neck incision. It has an excellent overall surgical success rate of up to 89%, which was defined as either the avoidance of tracheostomy or successful decannulation. EPCS/RG has been popularized for pediatric patients due to age-related changes in the cricoid cartilage’s stiffness and ossification, thus limiting its use in older patients.
“We found that with balloon dilation technique, endoscopic posterior cricoid grafting could be done with ease in an older age group, even with age-related changes in the cartilage,” Dr. Aldriweesh said. “The pressure of the balloon helped in dilating the posterior cricoid split and in locking the graft in place.” Another benefit, she added, was a faster operative time. She said other novel uses for balloon dilation are in oropharyngeal and hypopharyngeal stenosis management.
BDET with Laser Myringoplasty for Tympanic Membrane Atelectasis
Maggie M. Mouzourakis, MD was the lead resident speaker at the 2023 Triological Society Sections Meetings for a presentation on the role of BDET as an adjunct procedure for laser myringoplasty treatment of tympanic membrane atelectasis. Dr. Mouzourakis is a PGY3 at Dartmouth-Hitchcock Medical Center in Lebanon, New Hampshire; her mentor, Dr. Saunders, was the lead researcher.
Prior to the invention of balloon dilation, patients who had chronic dilatory Eustachian tube dysfunction, or difficulty equalizing pressure in their middle ears, had few options. —Maggie M. Mouzourakis, MD
“This is of particular interest to anybody in otology, I think,” Dr. Mouzourakis said, “because prior to the invention of balloon dilation, patients who had chronic dilatory Eustachian tube dysfunction, or difficulty equalizing pressure in their middle ears, had few options. We were frequently placing ear tubes, sometimes as often as every two years, because they [ear tubes] can become clogged, fall out, or have other complications.
Additionally, each time a new set of ear tubes is placed, the incision made in the eardrum can make the area weaker over time and cause scarring, with a recurring risk of a permanent tear. Balloon dilation, on the other hand, gets around the problem of repeated trauma and potential scarring to the eardrum while at the same time addressing at the source the inability to equalize pressure in the Eustachian tube.
Tympanic membrane atelectasis, when the eardrum becomes weaker over time and can withdraw into the middle ear space, forming cysts called cholesteatoma, can erode the bones in the ear as well as the bones that separate the ear from the brain and surrounding structures. “Using balloon dilation, we can address issues with chronic dilatory Eustachian tube dysfunction or negative pressure over time,” Dr. Mouzourakis said.
In patients with dilatory Eustachian tube dysfunction, laser myringoplasty can be done in conjunction with tympanostomy tubes to equalize pressure. “We thought that it might be interesting to see how laser myringoplasty patients fared with balloon dilation as an adjunct procedure to address the cause of tympanic membrane retraction, the dilatory Eustachian tube dysfunction,” Dr. Mouzourakis said, adding that Dr. Saunders usually does the balloon dilation procedure first, followed by laser myringoplasty in the operating room.
Preliminary results showed that balloon dilation may be equivalent to placement of tympanostomy tubes, can help prevent further procedures, and are also equivalent in terms of the researchers’ ideological outcomes. Because there weren’t many patients in the cohort study, this is an area that needs further research, Dr. Mouzourakis said, as it may be very useful in the future for patients with tympanic membrane atelectasis. She added that there has been very little research on the use of Eustachian tube balloon dilation for patients who have middle ear problems, tympanic membrane atelectasis, or adhesive otitis media, and for patients who are undergoing tympanoplasties.
“This is an area that’s still being discovered,” she said, “so I think it was just interesting to be able to explore that and be in the forefront of the field to see if this is something that can be useful so that we can prevent people from needing many, many sets of ear tubes.”
While the small study did not show a definite benefit to using BDET over tympanostomy tubes, Dr. Saunders said it does seem to be at least equivalent and has many potential advantages. “I think the biggest caveat is that not all patients with chronic ear disease have active Eustachian tube dysfunction. On the other hand, some of these patients may have dilatory dysfunction that’s too severe to be effectively treated with BDET.” He recommended being selective in choosing which patients might benefit from BDET alone.
Based on the preliminary research from this study, Dr. Mouzourakis said one of the big takeaways was that BDET is a very reasonable adjunct option for patients who have dilatory Eustachian tube dysfunction and tympanic membrane atelectasis and can potentially be equivalent to tubes.
“It’s something to definitely consider and counsel patients about,” she said.
Renée Bacher is a freelance medical writer based in Louisiana.
BDET Best Practices
According to Dennis Poe, MD, PHD, a professor of otolaryngology at Harvard Medical School and Boston Children’s Hospital, the following are best practices when considering balloon dilation Eustachian tuboplasty.
- Accurate diagnosis of obstructive Eustachian tube dysfunction. One of the main symptoms is aural fullness, but there are several other conditions that can cause this symptom, and it isn’t always easy to make sure this is true obstructive Eustachian tube dysfunction.
- Optimal medical management. Be sure the underlying medical condition (for instance, allergic disease) has been adequately treated and controlled.
- Appropriate patient selection. Be sure you’re picking patients who will be good candidates for this procedure. Someone with a chronic disease that isn’t in remission (e.g., aspirin-exacerbated respiratory disease) has a mucosal disease that the balloon won’t help.
- Don’t overtreat. Be sure the balloon treatment is commensurate with the severity of the pathology.
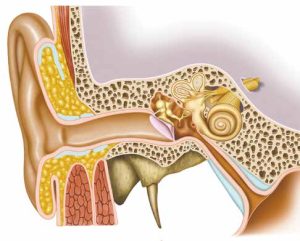
- Understand complication risks. Think ahead to avoid complications, and be aware of adjacent neurovascular structures—for example, make sure the balloon doesn’t get into the bony part of the Eustachian tube near the carotid artery, and insert the balloon slowly so you don’t get a false passage.
- Justify the expense. This is an expensive treatment, and insurance companies are all over the place on coverage. You may need to explain why the patient is not a good candidate for tympanostomy tubes. The perfect case is someone who has already had tubes that have fallen out.