Main Point
This case series describes the presentation, clinical course, and outcomes of six patients who underwent endoscopic revision stapes surgery. The results suggest that endoscopic revision stapes surgery is feasible and may provide a platform for a larger study to validate the efficacy of this approach with long-term outcomes.
Explore This Issue
September 2020Introduction
When compared to primary stapes surgery, revision stapes surgery has been reported to result in less favorable surgical and audiologic outcomes, with an increased risk of postoperative sensorineural hearing loss (SNHL) (Otol Neurotol. 2010;31:875–882). Due to the presence of altered anatomy, adhesions, and a previously manipulated oval window, revision stapes surgery is technically challenging. Prior studies have shown that the most common causes of failure after primary stapes surgery include prosthesis dislocation, short or long prosthesis, incus erosion or dislocation, perilymphatic fistula, and ankylosis of the lateral ossicular chain (Otol Neurotol. 2010;31:875–882. Otol Neurotol. 2011;32:373–383. Otol Neurotol. 2009;30:1092–1100. Otol Neurotol. 2006;27(suppl 2):S25–S47) The success of revision stapes surgery relies on intraoperative identification of the cause for initial surgical failure because a lack of diagnosis has been correlated with negative outcomes (Laryngoscope. 2018;128:2390–2396). Consequently, adequate visualization and evaluation of the ossicular chain and oval window are essential to accurately diagnose and treat the cause of failure.
An endoscopic approach to stapes surgery allows for enhanced visualization of the ossicular chain and oval window (Otol Neurotol. 2016;37:362–366. Laryngoscope. 2014;124:266–271. Otolaryngol Clin North Am. 2016;49:1215–1225. Otol Neurotol. 2018;39:1095–1101). Additionally, endoscopy of the middle ear has been especially useful in diagnosing ossicular malformations (Eur Arch Otorhinolaryngol. 2016;273:1723–1729), perilymphatic fistulas (Acta Otolaryngol Suppl. 1994;514:63–65), and ossicular fixation (Int J Pediatr Otorhinolaryngol. 2017;96:21–24. Otol Neurotol. 2016;37:1071–1076).
Although prior studies have demonstrated similar audiologic and surgical outcomes between endoscopic and microscopic approaches for primary stapes surgery (Laryngoscope. 2014;124:266–271. Otol Neurotol. 2017;38:662–666. Otolaryngol Head Neck Surg. 2016;154:1093–1098), endoscopic outcomes for revision stapes surgery have not been previously reported. This case series describes the presentation, clinical course, and outcomes of six patients who underwent endoscopic revision stapes surgery.
Preoperative Demographics and Intraoperative Findings
| Patient | Age | Sex | Ear | Prior Stapes Surgery (n) | Preoperative CT Findings | Intraoperative Findings | Intervention | Prosthesis | Postoperative Complications |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 47 | F | L | 1 | Displaced prosthesis | Displaced prosthesis | Laser stapedotomy, longer prosthesis | Nitinol piston | - |
| 2 | 63 | F | L | 1 | - | Missing prosthesis, Incus necrosis | Laser stapedotomy, longer prosthesis | Nitinol piston (malleus to fenestra) | - |
| 3 | 82 | F | L | 1 | Normal prosthesis positioning | Displaced prosthesis, prolapsed facial nerve | Laser stapedotomy, longer prosthesis | Nitinol piston | Temporary dysgeusia |
| 4 | 19 | F | L | 1 | - | Short prosthesis without incus contact | Laser stapedotomy, longer prosthesis | Nitinol piston | - |
| 5 | 57 | M | R | 3 | - | Displaced prosthesis, malleus fixation, incus necrosis | Laser stapedectomy, longer prosthesis | Titanium bucket handle | - |
| 6 | 51 | M | L | 1 | Displaced prosthesis only | Displaced prosthesis, oval and round window otosclerosis | Stapedectomy, oval window drill-out | Titanium bucket handle | Labyrinthitis resolved with steroids |
| CT = computed tomography; F = female; L = left. |
CT = computed tomography; F = female; L = left.
Methods
Following institutional review board (IRB) approval (IRB 171214, 022012-060.2), a retrospective chart review was performed of all adult patients who underwent endoscopic stapes surgery at two tertiary care otologic centers between 2014 and 2017. Patients who had a history of prior stapes surgery who underwent totally endoscopic revision stapes surgery were included in the study (three patients from each institution).
Patient demographics, clinical course, and audiologic data—including unaided air conduction thresholds, bone conduction (BC) thresholds, and speech discrimination scores—were recorded from the medical record. For each case, the cause of surgical failure was identified intraoperatively. Postoperative outcome variables included postoperative complications, prosthesis extrusion, dysgeusia, and tympanic membrane (TM) retraction or perforation. All patients had preoperative and at least six weeks of postoperative audiologic data. Audiometric testing and calculations were conducted as previously described (Otolaryngol Head Neck Surg. 2016;154:1093–1098). Audiometric data herein are presented according to the 1995 American Academy of Otolaryngology–Head and Neck Surgery consensus guidelines. Postoperative SNHL was defined as an increase in average unaided BC thresholds (at 500 Hz, 1000 Hz, 2000 Hz, and 4000 Hz) > 15 dB HL.4
An endoscopic approach to stapes surgery allows for enhanced visualization of the ossicular chain and oval window. Additionally, endoscopy of the middle ear has been especially useful in diagnosing ossicular malformations, perilymphatic fistulas, and ossicular fixation.
Surgery under general anesthesia was performed by two surgeons at two institutions. Patients underwent either stapedotomy or stapedectomy, which was dependent on the intraoperative findings, prior surgical history, and surgeon preference. The techniques for endoscopic stapedotomy and stapedectomy have been previously described (Otolaryngol Head Neck Surg. 2016;154:1093–1098. Curr Opin Otolaryngol Head Neck Surg. 2016;24:388–394. Otolaryngol Clin North Am. 2018;51:415–428). Patients who underwent laser stapedotomy received an Eclipse nitinol piston prosthesis (Grace Medical, Memphis, Tenn.), whereas those who underwent a laser stapedectomy received a titanium notched bucket handle prosthesis (Grace Medical) in conjunction with a perichondrial graft to seal the oval window after partial or total removal of the stapes footplate. In cases of incus necrosis precluding prosthesis placement on the incus, an Eclipse nitinol malleus to fenestra piston prosthesis (Grace Medical) was used.
Statistical analyses were performed with GraphPad Prism 7.0 (GraphPad Software, La Jolla, Calif.). Continuous variables were reported as medians with ranges when not normally distributed. Mann-Whitney testing was applied to medians with nonparametric values, with all tests two sided and P values less than 0.05 considered statistically significant.
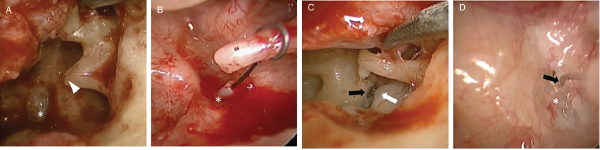
Fig. 1. Intraoperative findings. (A) Necrosis of long process of incus (arrowhead) resulting in prosthesis displacement from stapes footplate (*) (patient 2). (B) Prosthesis displaced to posterior rim of footplate (*) (patient 1). (C) Prosthesis displacement (removed) with prolapsed facial nerve (white arrow) and prominent bony overhang (black arrow), which was drilled to allow for prosthesis placement during revision surgery (patient 3). (D) Short wire loop prosthesis (black arrow) making poor contact with stapes footplate (*) (patient 4).
Results
Patient Characteristics
Between 2014 and 2017, a total of six adult patients with median age of 53.2 years (range, 19.1–82.6 years) underwent total endoscopic revision stapes surgery. All patients had an initial diagnosis of otosclerosis prior to primary stapes surgery, which in all cases was performed by a different surgeon. One patient had a history of three prior stapes surgeries of the ipsilateral ear, whereas the remaining patients had a history of a single prior stapes surgery. Prior to revision surgery, four (66.7%) patients reported tinnitus, whereas none reported dizziness. Patients 3 and 6 had a history of tobacco use. Three patients had preoperative imaging; the cause of failure was accurately diagnosed by computed tomography (CT) scan in one case (patient 1).
Surgical Technique
Each patient underwent transcanal totally endoscopic ear surgery (TEES) with the use of 0° and/or 30° endoscopes (100% and 33.3%, respectively). The endoscopic approach to the middle ear, including TM elevation, has been previously described (Otolaryngol Clin North Am. 2018;51:415–428). For revision stapes surgery, the integrity and mobility of the ossicular chain and prior prosthesis was first evaluated with palpation and visual inspection for bony erosion. Next, the prosthesis was evaluated for appropriate placement, size, and contact with the stapes footplate or graft overlying the oval window in the case of previous stapedectomy. Finally, the oval window was evaluated for progressive otosclerotic plaque, prolapsed facial nerve, or prominent bony overhang that could prevent ideal placement of a new prosthesis. Once the cause of failure was identified and addressed, the new prosthesis was placed using either a stapedotomy or stapedectomy technique.
Audiologic Outcomes, by Patient
| AC PTA, dB HL | BC PTA, dB HL | ABG, dB HL | SDS, % | |
|---|---|---|---|---|
| Patient 1 | ||||
| Preoperative | 47.5 | 16.3 | 31.3 | 100 |
| Postoperative | 33.8 | 20 | 13.8 | 90 |
| Change | -13.7 | 3.7 | -17.5 | -10 |
| Patient 2 | ||||
| Preoperative | 82.5 | 38.8 | 43.8 | 90 |
| Postoperative | 35 | 18.8 | 16.3 | 100 |
| Change | -47.5 | -20 | -27.5 | 0 |
| Patient 3 | ||||
| Preoperative | 95 | 66.3 | 28.8 | 22 |
| Postoperative | 75 | 66.3 | 8.8 | 42 |
| Change | -20 | 0 | -20 | 20 |
| Patient 4 | ||||
| Preoperative | 57.5 | 22.5 | 35 | 100 |
| Postoperative | 16.3 | 5 | 11.3 | 100 |
| Change | -41.2 | -17.5 | -23.7 | 0 |
| Patient 5 | ||||
| Preoperative | 65 | 25 | 41.7 | 100 |
| Postoperative | 63.8 | 21.3 | 42.5 | 100 |
| Change | -1.2 | -3.7 | 0.8 | 0 |
| Patient 6 | ||||
| Preoperative | 90 | 65 | 25 | 68 |
| Postoperative | 91.3 | 70 | 21.3 | CNE |
| Change | 1.3 | 5 | -3.7 | - |
| AC = air conduction; BC = bone conduction; CNE = could not examine; HL = hearing level; PTA = pure-tone average; SDS = speech discrimination score. |
AC = air conduction; BC = bone conduction; CNE = could not examine; HL = hearing level; PTA = pure-tone average; SDS = speech discrimination score.
Intraoperative Findings
Three patients (50%) had evidence of prior scutum removal. An additional two cases with an intact scutum required removal for visualization and instrumentation. The chorda tympani nerve was previously transected in two cases, required manipulation without transection in two cases, and was not manipulated in the remaining two cases.
Intraoperative endoscopic inspection of the middle ear revealed a displaced, loose, or missing prosthesis in all cases. Incus necrosis was noted in two cases (33.3%). Four patients (66.7%) underwent laser stapedotomy; one patient underwent laser stapedectomy; and one patient required an oval window drill-out due to extensive oval window involvement of otosclerosis. One case (patient 5) revealed malleus fixation, which was resolved with the release of an ossified anterior malleolar ligament and a medial malleus bar using a laser and right-angle pick. Surgical technique and treatment of the oval window were dependent on both middle ear anatomy and surgeon preference. The median operative time was 111 minutes (range, 84–154 minutes). There were no instances of intraoperative complications including TM perforation, floating footplate, facial nerve injury, or incus dislocation. All patients were discharged on the day of surgery without readmissions.
Audiologic and Surgical Outcomes
The median audiologic follow-up was 7.4 months (range, 1.5–33.3 months). At the time of last follow-up, the median air–bone gap (ABG) was 15 dB HL (range, 8.8–42.5 dB HL), improved from 33.1 dB HL (range, 25–43.4 dB HL) preoperatively (P < 0.0306). Five of six patients had a reduction in the ABG, whereas one patient (patient 5) had an increase of 0.8 dB. Overall, 66.7% of patients had a closure of the ABG to ≤20 dB.
Patient 6 experienced a temporary 20 dB SNHL hearing loss and vertigo one week after surgery. This patient was diagnosed with labyrinthitis and treated with a high-dose prednisone taper followed by resolution of symptoms and SNHL within three weeks. Postoperatively, patient three, who intraoperatively had manipulation but preservation of the chorda tympani nerve, reported dysgeusia that resolved within three weeks. Overall, there were no instances of permanent postoperative SNHL >15 dB HL, facial nerve injury, or TM perforations.
Discussion
The purpose of this study is to present the authors’ technique and results in applying an endoscopic approach to revision stapes surgery. Five out of six patients had an improved ABG, and two-thirds of patients had closure of the ABG to ≤20 dB. Although a small case series, these results are comparable to a large review of microscopic revision stapedotomy, which noted an ABG closure of ≤20 dB in 74.6% of cases (Otol Neurotol. 2010;31:875–882). Of the six cases included in this series, there was one case of postoperative labyrinthitis that resolved with a steroid course, and one case of postoperative dysgeusia that self-resolved within three weeks. Patient 5 was noted to have malleus fixation that was addressed intraoperatively; it is possible that recurrence of malleus fixation may account for a lack of improvement in postoperative ABG; however, this has not been confirmed.
Proponents of the endoscopic approach for primary stapes surgery cite enhanced visualization of the oval window and ossicles, with resultant improvement in diagnostic accuracy, as a primary advantage of the approach (Eur Arch Otorhinolaryngol. 2016;273:1723–1729. Int J Pediatr Otorhinolaryngol. 2017;96:21–24. Otol Neurotol. 2016;37:1071–1076). These same advantages apply to revision stapes surgery for surgeons already routinely performing totally endoscopic stapes surgery. In this series, all patients presented for revision surgery after having primary surgery performed elsewhere. For patients who have had prior surgery and variably altered anatomy, an endoscopic view can provide enhanced visualization of the oval window, prosthesis, and the lateral chain.
Importantly, success in revision stapes surgery is correlated with an accurate diagnosis of the cause of failure (Laryngoscope. 2018;128:2390–2396). For example, the extent of incus necrosis dictates repair options and ultimately clinical outcomes (J Int Adv Otol. 2017;13:28–31). A close analysis of the incus and accurate evaluation of the extent of necrosis requires excellent visualization of the ossicular chain. Similarly, malleostapedotomy requires detailed visualization and inspection of the oval window and lateral ossicular chain; the endoscopic approach has been applied in this setting and shown to be effective in a small case series (Laryngoscope. 2018;128:2611–2614). Notably, the cause of surgical failure was accurately diagnosed with imaging in one of three patients who had preoperative CT scans; however, conclusions regarding the utility of preoperative CT scans cannot be drawn from this small sample size.
Conclusion
Because TEES is more widely adopted, this approach will be explored in new applications. For the surgeon who is using TEES in other cases, an endoscopic approach in revision stapes surgery may provide advantageous visualization and diagnostic accuracy. The results of this small case series suggest that endoscopic revision stapes surgery is feasible and may provide a platform for a larger study to validate the efficacy of this approach with long-term outcomes.