How will biologic response modifiers change the treatment paradigm for patients with chronic rhinosinusitis with nasal polyposis? Otolaryngologists now have an expanded treatment armamentarium along with conventional surgical treatment, as new, immunomodulating drugs are approved to treat this condition.
Explore This Issue
November 2019Biologics target and suppress specific drivers of inflammation in the immune system. They may work well in some patients to treat the symptoms of nasal polyps, but high cost and the need for regular injections for an indefinite period of time are two major concerns among otolaryngologists. Most patients experience significant symptom relief with complete surgical polypectomy followed by topical corticosteroid irrigation, they say.
Dupilumab Approved in 2019
In June 2019, dupilumab (Dupixent, Sanofi Genzyme) was approved by the U.S. Food and Drug Administration (FDA) to treat adults with nasal polyps accompanied by chronic rhinosinusitis. In the announcement of the drug’s approval for this indication, Sally Seymour, MD, director of the division of pulmonary, allergy and rheumatology products in the FDA’s Center for Drug Evaluation and Research, said that dupilumab “provides an important treatment option for patients whose nasal polyps are not adequately controlled with intranasal steroids. It also reduces the need for nasal polyp surgery and oral steroids.”
Other biologics are being studied in clinical trials for treatment of nasal polyps, including omalizumab (Xolair, Novartis) and mepolizumab (Nucala, GSK). Each targets a different inflammatory trigger (see “Biologics: Inflammatory Targets,” below). Biologics like dupilumab have already been approved for other indications, such as asthma and eczema. How do they work in patients with sinusitis and nasal polyps? Otolaryngologists have mixed views on their efficacy when compared with the conventional treatments of surgery and steroid irrigation.
“Biologics are highly targeted therapies to treat the inflammatory cascade in a subset of patients. But we don’t know which patients. Because they are targeted, there is a need for selective criteria to know which patients would benefit from this treatment. What we have are clinical trials run by pharmaceutical companies in a highly selective group of patients,” said Benjamin S. Bleier, MD, Claire and John Bertucci Chair in Otolaryngology/Head and Neck Surgery at Harvard Medical School in Boston. “There are several biologics on the market, and more are coming. We expect general efficacy, but when these drugs are prescribed across the patient spectrum, they may be less effective.”
Enthusiasm with Caution
Allergists have more enthusiasm for their effectiveness in patients with nasal polyps, which is estimated at 2.7% of the adult population, with higher prevalence in males, those older than 60, and people with asthma (Ann Otol Rhinol Laryngol. 2003;112:625–629).
Dupilumab “has shown close to magical success, with a patient response within two to four weeks of treatment. They are breathing better through their nose and regaining a sense of smell. For patients with severe asthma and nasal polyps, the response has often been quite remarkable,” said Tanya M. Laidlaw, MD, assistant professor of medicine at Harvard Medical School and director of translational research in allergy at Brigham and Women’s Hospital in Boston.
The pros of these drugs include that they help people avoid the use of long-term steroids. But the cons are that they’re very expensive and require lifelong injections every two to four weeks. —Rodney J. Schlosser, MD
Biologics like dupilumab, which suppress the immune system, have potential side effects, Dr. Laidlaw added. Dupilumab’s possible adverse effects include allergic reactions, conjunctivitis, keratitis, injection site reactions, eye and eyelid inflammation, eosinophilia, insomnia, toothache, arthralgia, and gastritis. Patients must not receive live vaccines while taking the drug. However, she has seen only mild reactions from her patients on dupilumab.
“So far, we have not come up against an infection issue with this drug. Local rashes in some patients, and I had a couple of eosinophil counts go up, so we follow these patients. But patients have begged me not to go off their drug. For patients who have failed other treatments, this drug has been incredibly life-altering for them,” she said. “Right now, in part because of knowledge of short- and long-term side effects and costs, if a single surgery gives you five to 10 years of relief, it may be worthwhile to have surgery every five to 10 years. My approach to this is that in patients who have already had one surgery, and either have polyp recurrence after surgery or if the surgery didn’t improve their symptoms enough, then I think dupilumab is a good choice.”
Better for Severe Polyps
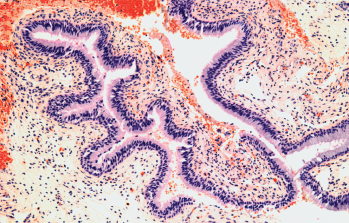
Light micrograph of a section through a nasal polyp.
© STEVE GSCHMEISSNER / Science Source
Biologics may be more appropriate in patients with severe polyps than in those with mild to moderate polyps, said Rodney J. Schlosser, MD, director of the Nose and Sinus Center at the Medical University of South Carolina in Charleston. He finds dupilumab’s clinical trial results encouraging, and feels the new drug has good outcomes for quality of life and polyp score reduction.
“Biologics have been studied primarily in patients with severe polyps based on grading scores, but they have not been studied in patients with mild to moderate polyps,” said Dr. Schlosser. “The pros of these drugs include that they help people avoid the use of long-term steroids. But the cons are that they’re very expensive and require lifelong injections every two to four weeks. Injections would be required indefinitely. Biologics should be reserved for patients who have failed comprehensive sinus surgery followed by postoperative steroid rinses. That treatment controls the vast majority of polyp patients. Most don’t need a revision surgery. In the past, surgeons did repeated polypectomy. Now, we know that comprehensive polyp surgery is required to really open the sinuses, and then we deliver the steroid rinse.”
How expensive are biologics? While out-of-pocket costs vary considerably depending on a patient’s individual insurance coverage, dupilumab’s average wholesale price for one box of two prefilled 300 mg/2 mL syringes is $3,517.85, and its wholesale acquisition cost (WAC) is $37,000 per year (P.T. 2018;43:532–535). Endoscopic sinus surgery costs also vary widely depending on location, center, and insurance coverage, but one estimate of the mean cost for surgery is around $10,000 (Value Health. 2018;21(suppl 1):S13).
Not Enough Shrinkage
Biologics may also shrink, but not remove, polyps as thoroughly as surgery, Dr. Schlosser said. “On the grading scale of zero to eight, biologics improve them from 5½ to 3½, from severe to moderate. And there are some patients who have no change in polyp score with biologics, so there appear to be some people who do not respond. Physicians have to weigh the options and help the patient make the right decision based on the individual’s needs and comorbidities.”
Symptoms, not grading systems, guide physicians’ assessment of polyp severity and help identify who may be a good biologics candidate, said James N. Palmer, MD, a professor of otorhinolaryngology–head and neck surgery at the Hospital of the University of Pennsylvania in Philadelphia.
“Patients usually have chronic sinusitis if they have pressure, pain, headaches, nasal obstruction, nasal drainage, and a decreased sense of smell,” said Dr. Palmer. “Surgical removal and application of a topical steroid works well to remove the polyps or keep them from coming back. A large proportion of patients do really well with this treatment. But they need to have complete, not partial, surgery. They also need to do steroid irrigation washes as a lifelong treatment. But most patients will comply to avoid another surgery.”
Biologics Right for Subset of Patients
After complete surgery and topical steroid application, polyps often do not recur. This treatment provides significant improvement in nasal symptoms and improves the patient’s asthma, but does not cure it, said Dr. Palmer. Patients with polyps who have poorly controlled asthma may be treated with either oral corticosteroids or biologics, he added.
“Dupilumab works in a large percentage of patients, in my opinion, while complete surgery and steroid irrigation will control it in many more. However, biologics may be right for certain subsets of patients. One, patients who want or need to avoid surgery for some reason. Two, patients who have a good surgery and topical steroid treatment, but the asthma is not controlled by topical therapies,” he said. “We are working toward identifying endotypes. All polyps have inflammatory triggers and different underlying genetic conditions that drive the development of the polyps.”
For patients who have failed other treatments, this drug has been incredibly life-altering. —Tanya M. Laidlaw, MD
Biologics may be the right option for patients whose polyps do recur, after eliminating those who may have had either incomplete surgical removal or incomplete post-surgery medical management with steroids, said Timothy L. Smith, MD, MPH, professor of otolaryngology–head and neck surgery in the division of rhinology and sinus surgery at Oregon Health and Science University in Portland.
“It’s in that population that we are particularly interested in newer, better treatments. Enter the biologics. These block the molecules that are possibly involved in the inflammation. We are becoming better at identifying inflammatory mediators, but you still don’t know which specific inflammatory molecule you need to block in each specific patient. Some patients have responded dramatically to these drugs, but some have little or no response,” said Dr. Smith, who added that there may be 100 or more inflammatory pathways involved in polyp development.
Patients with aspirin-exacerbated respiratory disease are one group who would likely benefit from biologics, as they are known for high polyp recurrence rates, said Dr. Palmer. “Their polyps can come back quickly. These patients often require ‘big hole’ surgery to get all the polyps out, followed by strong steroid irrigation. Recurrence of polyps after complete surgery, steroid irrigation, and aspirin desensitization is at best 10% at three years, and in this recalcitrant group, biologics would mostly fit well,” he said.
Dupilumab and other biologics may be more appropriate for patients after surgery and steroid irrigation has failed, but not as a first-line treatment, said Dr. Palmer. While biologics seem relatively safe, they still modulate a patient’s immune system and must be used indefinitely. “Still, surgery is a time-honored treatment with low side effects. If a patient’s symptoms come back, then I would consider biologics. Biologics give us another piece in our armamentarium of treatment.”
Surgery is a time-honored treatment with low side effects. If a patient’s symptoms come back, then I would consider biologics. Biologics give us another piece in our armamentarium of treatment. —James N. Palmer, MD
Shared Decision Making
Will otolaryngologists feel threatened by the emergence of biologics that reduce the number of sinus surgeries? This is a natural response, “but also a completely inappropriate way for us to respond to new treatments and technologies that may benefit our patients,” says Dr. Smith. “We have a potential conflict of interest as sinus surgeons. Our allergy/immunology colleagues have a potential conflict of interest as well. The worst thing we can do is put our patients in the middle of our conflicts of interest.”
Dr. Laidlaw, an allergist, said she works in a multidisciplinary manner with surgeons in her health system, so patients are referred to the right clinician for treatment appropriate for their situation.
Dr. Smith agreed. “This highlights the need for multidisciplinary management of this patient population. None of us has all the tools. We need to work together,” he said. “This issue really pushes the paradigm of multidisciplinary collaboration, and that’s where we should take this, almost like tumor boards in cancer treatment. We can make recommendations to patients as a multidisciplinary group.”
Susan Bernstein is a freelance medical writer based in Georgia.
Key Points
- Biologics target and suppress specific drivers of inflammation and work well in some patients to treat the symptoms of nasal polyps.
- Cost and the need for regular injections for an indefinite period of time are two major concerns among otolaryngologists.
Biologics: Inflammatory Targets
Biologics suppress inflammation, so the argument in favor of these drugs is that they will be more effective in patients with poorly controlled, severe nasal asthma and polyps that are inflammation-driven, but there are still many unknowns about these drugs in this patient population, said Dr. Bleier.
“If you have a patient who is struggling with asthma control, has severe polyps, and is a poor surgery candidate, they may be a good biologics candidate. We always have to balance the cost of therapy and the true efficacy of therapy,” he said. “Because these drugs are very new, in addition to unknown efficacy across the general spectrum of patients, we don’t know if there will be a rebound effect, or if there is better efficacy in treatment-refractory patients.”
Dr. Bleier describes polyps as “bags full of inflammatory products,” or cytokines that are targeted by biologics. Once polyps are surgically removed, he wonders if biologics may work better, because “the cytokines are already reduced.”
Which cytokines do the new crop of biologics target?
- Dupilumab (Dupixent, Sanofi Genzyme) is a monoclonal antibody that targets the alpha chain of the IL-4 receptor and inhibits the effects of IL-4 and IL-13, two cytokines involved in inflammation in chronic sinusitis with nasal polyposis.
- Mepolizumab (Nucala, GSK) is a humanized anti-IL-5 antibody that has also been shown to significantly reduce nasal polyps and improve smell, post-nasal drip, and nasal congestion.
- Omalizumab (Xolair, Novartis) is a fully humanized, anti-IgE monoclonal antibody that has also been shown to significantly reduce polyp size and improve symptoms in clinical trials (Allergy Clin Immunol Pract. 2016;4:565–572).
At this time, mepolizumab and omalizumab are not approved for treatment of nasal polyposis. Other biologics being studied for nasal polyp treatment include two other monoclonal antibodies, reslizumab (Cinqair, Teva) and benralizumab (Fasenra, AstraZeneca) (Am J Rhinol Allerg. 2019;33:203–211).