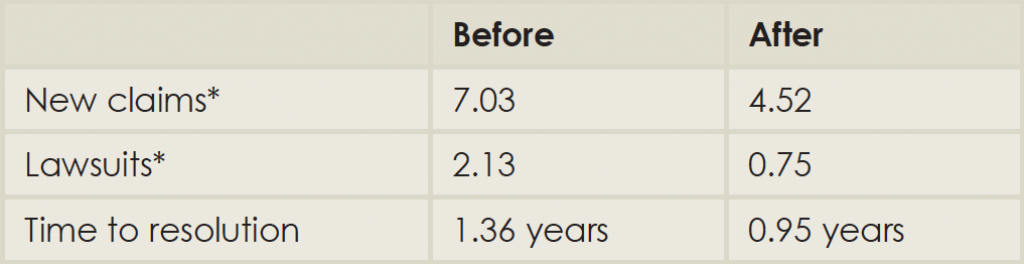
Comparison of Malpractice Claims before and after Implementation of the Michigan Model
(Click for larger image)
*Numbers reported are per month per 100,000 patient encounters.
Source: Adapted from Ann Intern Med. 2010;153:213-221.
The apology part of the process is difficult. It goes against one’s instincts, especially a physician who has practiced in a setting where mistakes are not generally permitted. Boothman once counseled an oncologist after a breast cancer diagnosis was delayed. They talked about the impact of the delay, and discussed sitting with the patient and the plaintiff’s lawyer. Boothman quoted the physician: “I would rather eat tacks.”
Explore This Issue
July 2015Dr. Damrose advises keeping the safety goals in mind. “When we’re talking to the patient and the family, we’re telling them what we learned from this and what changes we will put in place,” he said. Listening is equally crucial. The family sometimes simply needs to be heard, he added. “Sometimes they need to vent.”
Both Michigan and Stanford keep their physicians informed about the disclosure protocols: how to report an adverse event, whom to talk to, where to find support. Residents and faculty from other institutions undergo an orientation for the communication and resolution programs; current faculty get periodic refreshers at faculty meetings. Boothman reported that some incoming physicians have told him they came to Ann Arbor specifically because of the Michigan Model.
Both health systems also receive queries from other institutions. “I get maybe six calls a month,” Boothman said. He gets one of two responses from skeptics. Either he hears, “It could never happen here!” or “We’re already doing it.” “For years, physicians have been told to say nothing and let the risk management people deal with it,” Dr. Saint said. “We’ve been afraid to open ourselves up to lawsuits.”
The fear of being sued leads to some medical practices that have come under recent scrutiny, such as ordering up more tests and treatments so that the physician is protected from a frivolous lawsuit, said Dr. Saint.
The Michigan Model of communication and resolution is a huge departure from that tradition, but it also honors the medical creed: Do no harm. Rather than avoiding risk of lawsuits, it says physicians should avoid repeating mistakes. The reduction in malpractice claims and costs is simply a bonus. “The ultimate goal is to be open about the errors we make, to avoid making them again, and to avoid losing the trust of our patients and families,” said Dr. Saint.