Beth Drolet, MD, professor of dermatology and pediatrics at the Children’s Hospital of Wisconsin in Milwaukee, said much more research is needed. “Although there have been over 60 articles describing the use of this medication for treatment of infantile hemangiomas, there is very little data prospectively evaluating the toxicity of this drug in this population,” she said.
Explore This Issue
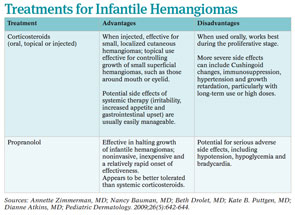
July 2011To fill the gap in the evidence on toxicity, a number of prospective, randomized clinical trials are currently recruiting patients to compare propranolol to corticosteroids (See “Prospective, Randomized Trials,” p. 4).
Need for Caution
Despite the lack of prospective data on toxicity, current data already indicate the need for caution when using propranolol in some infants and in specific situations.
Among the children who may be at the highest risk for side effects are the very young. “Physicians need to realize that some infants with infantile hemangiomas are preterm and low birth weight, which may put them at increased risk of side effects,” said Dr. Drolet. She was recently awarded federal funding to design a prospective trial that will compare toxicity and efficacy of prednisolone combined with propranolol and propranolol alone in infants with complicated hemangiomas.
A major and potentially dangerous possible side effect for these young infants is hypoglycemia, the biggest risk factor in infants under six months old, according to Kate B. Puttgen, MD, assistant professor of pediatric dermatology at Johns Hopkins University in Baltimore, Md., who added that this statement is based on anecdotal data and case studies (J Am Acad Dermatol. [Published online ahead of print May 19, 2011]).
To ensure proper monitoring in her patients, Dr. Puttgen admits most patients under 12 months so that she can monitor them for 48 hours to reach a dosing goal of 2 mg/kg/day divided by 8 hours (0.67 mg/kg/dose). For those infants being treated on an outpatient basis, she doses much more slowly, increasing to a target dose over 10 to 14 days. For all patients, she monitors blood pressure and heart rate until the infant is stable on the drug and also at each follow-up visit.

“Most infants need to be on the drug for six months or more,” she said. “They need to be treated at least until the hemangioma is beyond its natural proliferative phase.”
To prevent hypoglycemia, Dr. Bauman emphasized that physicians must educate parents about the need to keep their infants on a regular feeding schedule. This is particularly important when infants may stop eating because of a viral infection, for example.
Leave a Reply