Explore This Issue
September 2012Whatever the initial injury—stroke, Bell’s palsy or Ramsay Hunt syndrome, sacrifice of the nerve during tumor resection or traumatic injury—facial paralysis is often psychologically devastating to patients.
Despite an ever-increasing armamentarium of treatment approaches, misconceptions about treatment options and prognoses still exist, said Babak Azizzadeh, MD, FACS, director of the Facial Paralysis Institute in Beverly Hills, Calif. He vividly recalls seeing one patient who had suffered facial paralysis for almost a year, a man whose primary care physician had told him that there was “nothing we can do.”
Otolaryngologists who specialize in diagnosing and treating facial paralysis would like to combat that attitude. Advances in minimally invasive treatment and multidisciplinary approaches to this condition have resulted in restoration of symmetry and function, as well as better quality of life, for those affected.
The Eyes Come First
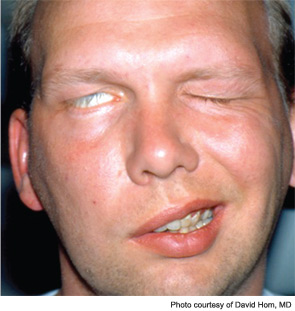
The most common acute presentation of facial paralysis is Bell’s palsy, thought to result from a polyneuritis of idiopathic etiology. A viral etiology (i.e., herpes simplex type 1, herpes zoster and others) has been suspected to play a role. Many recommend a trial course of steroids and possibly antivirals, although recent evidence has not supported the use of antivirals (N Engl J Med. 2007;357(16):1598-1607). Definitive attention to eye protective measures is imperative.
David Hom, MD, professor of otolaryngology and director of the division of facial plastic and reconstructive surgery at the University of Cincinnati College of Medicine, teaches an instructional course with a colleague on facial paralysis at the annual meeting of the American Academy of Otolaryngology-Head and Neck Surgery and emphasized that Bell’s palsy is a diagnosis of exclusion. Clinicians must rule out other causes of the paralysis, which could include stroke, acoustic neuroma, a parotid lesion or even Lyme disease, among other causes. Ravi N. Samy, MD, neurotology fellowship program director at the University of Cincinnati/Cincinnati Children’s Hospital Medical Center and co-instructor of the course, includes in his complete history questions about outdoor activities to assess the necessity for a Lyme titer; a screening hearing test may lead to a CT or MRI scan to rule out skull base pathology. For example, an imaging study on Dr. Azizzadeh’s patient revealed an acoustic neuroma that was later removed, and the patient made a full recovery.
Leave a Reply