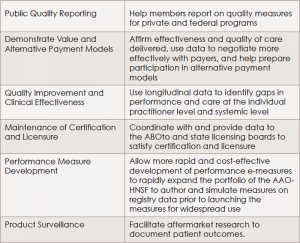
(click for larger image)Benefits Offered by Regent
ABOto, American Board of Otolaryngology; AAO-HNS, American Academy of Otolaryngology–Head and Neck Surgery
Source: AAO-HNS. Regent ENT Clinical Data Registry, available at:
entnet.org/content/otoregistry.
According to Dr. Weber, the data collected by Regent will come from critical data elements captured for and generated by general otolaryngology and each subspecialty within the field. It is anticipated that these data will be electronically extracted from the providers’ electronic medical records, he said.
Explore This Issue
April 2016Dr. Weber, who is leading the development of the practice improvement module for head and neck surgery, cited the example of capturing the critical data elements that relate to taking care of patients with head and neck tumors. “These data will include outcome measures and quality measures collected across a large group of patients with different types of head and neck cancers and will be risk adjusted,” he said.
Using the established measures of quality, physicians will then enter data on their patients’ outcomes electronically into the database and will be able to see how the outcomes of their patients compare to those of other physicians treating the same type of condition. For example, Dr. Weber said that one quality measure used in treating patients with head and neck cancer is determining whether physicians ask their patients about smoking history and whether they refer all patients who do smoke to resources to help them quit. “If a physician falls below 90% referral of patients for smoking cessation, the physician would want to implement some practice changes that would help him or her meet the quality standard of 90% or greater,” he said, adding that this may take the form of, for example, an intake nurse asking patients about smoking and incorporating an automatic trigger for a referral for patients who do smoke to the appropriate treatment resource.
Dr. Weber emphasized that as practice improvement modules within otolaryngology are developed, Regent will be able to transfer individual physician data to the practice improvement module electronically, without the need to manually extract the data from the patient’s chart and input it. “Our hope is to make this easier and decrease the burden on the practitioner to collect and report data,” he said.
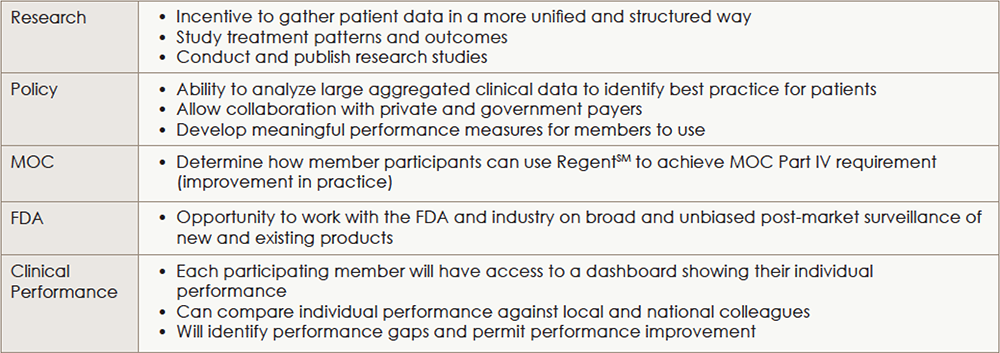
(click for larger image)
Main Uses for Collected and Aggregated Data
MOC, Maintenance of Certification; FDA, Food and Drug Administration.
This is also valuable in terms of part IV of maintenance of certification (MOC), he said, where data from Regent can be incorporated into the practice improvement modules and used as a quality improvement tool. During the current pilot phase, the AAO-HNSF has also applied to get approval for the database as a Qualified Clinical Data Registry (QCDR). Once certified as a QCDR, Dr. Ishii said that participating members can get credit for physician quality reporting system (PQRS).
Getting Otolaryngologists on Board
“Based on the initial great enthusiasm [more than 1,000 individuals reached out to participate in the pilot], and based on the experience of our peer organizations, we expect broad participation,” said Dr. Ishii. “Once members realize the benefits to participation in Regent, we fully expect that the vast majority of members will want to participate.” How many members will get on board will be better known once the pilot phase ends in late summer or early fall of 2016 and the database is officially launched and available to all members.