Explore This Issue
May 2014
Recently published data that adds to the accumulating evidence suggesting that the rapid rise in thyroid cancer represents an epidemic of diagnosis rather than disease is increasingly challenging otolaryngologists and other clinicians to rethink both the diagnosis and treatment of specific thyroid cancers—namely, small papillary thyroid cancers.
In their most recent study, which looked at the incidence of thyroid cancer diagnosed between 1975 and 2009 in the United States, Louise Davies, MD, MS, of the White River Junction VA Medical Center, and H. Gilbert Welch, MD, MPH, of the Geisel School of Medicine, Dartmouth College, Hanover, N.H., report that the incidence of thyroid cancer nearly tripled and that nearly the entire increase in thyroid cancer diagnoses was due to papillary thyroid cancer. Published online in JAMA in February 2014, the study confirms the findings reported by the investigators in 2006 in their first seminal study, which showed a doubling of papillary thyroid cancer diagnoses from 1975 to 2002, with 87% of the increase in tumors 2 cm or smaller. Using data from the Surveillance, Epidemiology, and End Results (SEER) Program and data on thyroid cancer mortality from the National Vital Statistics System, both studies also showed that during these years thyroid cancer mortality remained stable (see Table 1).
What emerged from these studies is a growing recognition among many clinicians of the overdiagnosis and subsequent overtreatment of thyroid cancers that will never cause symptoms or death. This recognition has created the need to address the overdiagnosis of thyroid cancer on two fronts: 1) reducing the number of small papillary cancers of the thyroid that are identified and 2) rethinking the management of biopsy-proven small papillary thyroid cancer.
Underlying this discussion is a strong recognition of the need to educate patients on the risks and benefits of diagnosing and treating these small papillary tumors, most of which will never create problems.
“Otolaryngologists are key in the solution to avoid overdiagnosis and overtreatment of thyroid cancer,” said Juan P. Brito, MBBS, Knowledge and Evaluation Research Unit, division of endocrinology, diabetes, metabolism, and nutrition, Mayo Clinic, Rochester, Minn. “Many patients with small papillary lesions receive therapies designed for more aggressive tumors. Otolaryngologists who are willing to avoid unnecessary therapies should incorporate the values and preferences of the patients in the decision-making process and start by telling patients what their options are and the advantages and disadvantages to each option.”
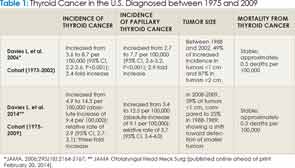
*JAMA. 2006;295(18):2164-2167; ** JAMA Otolaryngol Head Neck Surg [published online ahead of print February 20, 2014].
The Gauntlet Is Down: Toward a Patient-Centered Practice
According to Luc G. T. Morris, MD, an otolaryngologist on the head and neck service in the department of surgery at Memorial Sloan-Kettering Cancer Center, New York, N.Y., the real controversy for most otolaryngologists, and the area in which a consensus in the specialty is needed, is what to do with a patient who has a biopsy-proven cancer of a small nodule that should not have been biopsied.
Leave a Reply