Explore This Issue
November 2013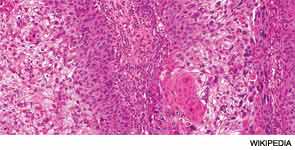
VANCOUVER—The number of skin cancer cases in the U.S. is growing, and a huge number of those patients are treated with Mohs microsurgery, often performed by dermatologists. But a panel of head and neck surgery experts at the 2013 AAH-HNS Annual Meeting said that there are times when Mohs surgery might not be appropriate and that it’s a procedure that can come with down sides.
There has been a nearly 250 percent increase in procedures performed for skin cancer, paralleled by a rise in treatment of the disease by dermatologists, primarily through procedures performed in their offices, said Christine Gourin, MD, MPH, the session moderator and associate professor of otolaryngology-head and neck surgery at Johns Hopkins University in Baltimore. “Primarily, this treatment is Mohs,” she said. The microsurgery approach has been embraced because it spares healthy tissue while eradicating cancerous tissue, due to examination of the tissue during the procedure rather than afterward.
“The difficulty,” Dr. Gourin said, “is that dermatologists do not read the same literature that we do.” An example is literature acknowledging that the value of sentinel lymph node (SLN) biopsy is supported by evidence. “[Dermatologists] don’t see it as the standard of care,” she said.
Divide in Care Approach
Derrick Lin, MD, co-director of the Cranial Base Center at the Massachusetts Eye and Ear Infirmary in Boston, discussed the difference in approach between the head and neck surgery community and the dermatological community. “That’s always a tough question.… Most head and neck surgeons [will] say, ‘Well, Mohs is never indicated.’ You talk to a dermatologist, and they’ll say it’s indicated for everything. So, it’s always a hard divide between the two subspecialties.”
The dermatology literature says that resection without Mohs encompasses only 60 percent of margins, while Mohs encompasses the entire margin, accounting for its growth in popularity.
The degree to which the dermatology community has embraced Mohs surgery, he said, can be seen in a statement issued in 2012 by a consensus group of dermatologic surgeons. The group looked at 161 primary articles from the previous 71 years, case series of more than three and case reports. They tabulated the data and held four rounds of discussion.
The result is a report that concludes that Mohs is seen as “almost appropriate for everything,” Dr. Lin said. Both in and outside of the “H zone,” the area of the face that is considered at higher risk, the only situation deemed inappropriate for Mohs was primary or recurrent actinic keratosis with squamous cell carcinoma in situ.
Leave a Reply