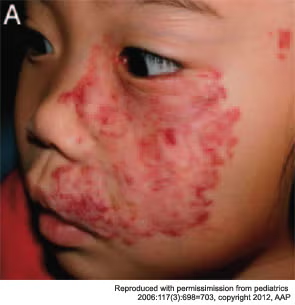
A bright red patch on the face of an infant might be a hemangioma, but what kind? A panel tackled the topic here on Jan. 26 at the Triological Society Combined Sections Meeting.
Explore This Issue
February 2012Stephen Conley, MD, a pediatric otolaryngologist at Children’s Hospital of Wisconsin, said hemangiomas in pediatric patients pose a special challenge because the proper way to proceed might not be clear immediately. “Their behavior has made it difficult to predict the need for treatment,” he said.
Carol MacArthur, MD, associate professor of otolaryngology-head and neck Surgery at the Oregon Health & Science University, urged biopsies when doctors aren’t sure about the type of a hemangioma. Congenital hemangiomas and other types may bear similarities to the less serious infantile hemangiomas, but there are key differences.
Maxillary segmental hemangiomas.

“They often initially look like an infantile hemangioma,” Dr. MacArthur said, “but on closer inspection have some differences and often act very differently. One of the main take-home messages I would like to convey is when things aren’t going in a typical fashion, think about doing a biopsy.” That will help differentiate infantile hemangioma, which are GLUT 1-positive, from the others, which are all GLUT 1-negative.
Rapidly involuting congenital gemangiomas (RICH) are fully formed at birth and rapidly collapse and fade within six to 12 months after birth, likely not needing medical therapy. But ulceration during involution might call for excising them earlier, Dr. MacArthur said.
Non-involuting congenital hemangiomas (NICH) are more rare, have a raised surface, and don’t respond to medical therapy. They might need to be excised, with embolization prior to the operation.
Kaposiform hemangioendothelioma (KHE) is a more aggressive, infiltrating vascular mass and can lead to Kasabach-Merritt Syndrome, which involves thrombocytopenia and microangiopathic hemolytic anemia and can have a mortality rate of up to 30 percent. Vincristine is most commonly used to treat these.
Tufted angioma can also lead to K-M Syndrome and treatment can include propranolol, although often at high doses, as well as vincristine and steroids.
Robert Yellon, MD, co-director of pediatric otolaryngology at the Children’s Hospital of Pittsburgh, said PHACES Syndrome, a neurocutaneous syndrome, is “underappreciated and underdiagnosed.” “When these occur, they’re important because the kids can be very sick because of cardiac and intracranial and vascular anomalies,” Dr. Yellon said.
Leave a Reply