In the wake of this year’s landmark health care reform legislation, one of the most hotly debated topics comes courtesy of the Dartmouth Atlas of Health Care (www.dartmouthatlas.org), as politicians, analysts, researchers and physicians grapple over how to resolve the contentious issue of geographical disparities in health care spending.
Explore This Issue
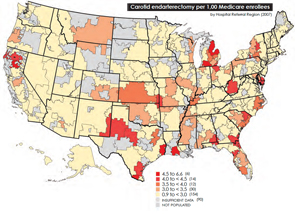
August 2010One of the main bodies of evidence driving the debate, the interactive Dartmouth map, depicts a color-coded nation in which wide swaths of the upper Midwest and West are colored with a pale yellow hue, which represents areas receiving significantly reduced amounts of Medicare reimbursement. Meanwhile, states such as California, New York, New Jersey, Massachusetts, Florida, Texas and Louisiana are marked by a darker shade of brown, which represents the nation’s most expensive per capita reimbursement rates.
The implicit message is that some states, cities and health providers have been shortchanged in their reimbursements—a complaint that flows into the larger meme that the country’s dysfunctional payment system rewards quantity, not quality. Officials at the Rochester, Minn.-based Mayo Clinic, for example, have suggested in media accounts that the current Medicare formula cost the clinic $840 million in lost reimbursements in 2008 alone, the result of what they deem inadequate rates that don’t reflect the true cost of care for older patients.
Health Reform Provisions
As part of negotiations leading to the passage of the health care reform package in March, a group of Democratic representatives calling themselves the Quality Care Coalition secured a pledge from the Department of Health and Human Services (HHS) to commission two studies on “unjustified geographic variation in spending and promoting high-value health care” and work toward a more evenly colored landscape (http://house.gov/wu/pdf/3.20.10_Sebelius_Letter_to_Quality_Care_Coalition.pdf).
The more than 50 legislators, hailing primarily from the Midwest and Pacific Northwest, initially pushed through the wording as a condition for supporting the House’s health care reform bill late last year. Their provisions weren’t included in the Senate’s health care bill or the reconciliation package, however, necessitating a round of negotiations with HHS to smooth the way for House Democrats to sign on to the final legislation.
One provision directs the nonpartisan Institute of Medicine (IOM) to check the accuracy of the geographic adjustment factors that underlie existing Medicare reimbursements and suggest necessary revisions. Guided by those findings, HHS Secretary Kathleen Sebelius will adjust the rates by Dec. 31, 2012. The second provision calls upon the IOM to conduct a study aimed at changing the Medicare payment system to reward value and quality. An Independent Payment Advisory Board will then use both studies to tweak the Medicare reimbursement rates a second time, by 2014. Secretary Sebelius has also agreed to convene a National Summit on Geographic Variation, Cost, Access and Value in Health Care sometime later this year.
Leave a Reply