BACKGROUND
Medullary thyroid carcinoma (MTC) comprises less than 5% of thyroid cancers but is responsible for more than 10% of deaths related to thyroid cancer. MTC arises from the calcitonin-producing parafollicular C cells. Most cases are sporadic (75%), although 25% are hereditary in people with multiple endocrine neoplasia type 2A and 2B. Regional lymph node metastasis is common and associated with mortality; thus, total thyroidectomy with central compartment (Level VI) lymph node dissection is the standard surgical treatment for MTC. However, the extent of prophylactic neck dissection (ND) of the lateral node compartments (Levels II-V) remains controversial when there is no clinical lymphadenopathy or radiographic evidence of nodal metastasis. Calcitonin is a sensitive biomarker for MTC, and there is evidence that pre-operative serum calcitonin predicts the presence and extent of lymph node metastasis. Given the postoperative morbidity and potential complications of ND, can calcitonin levels serve as a simple, cost-effective approach for risk-stratifying MTC without overt lymph node involvement?
Explore This Issue
October 2024BEST PRACTICE
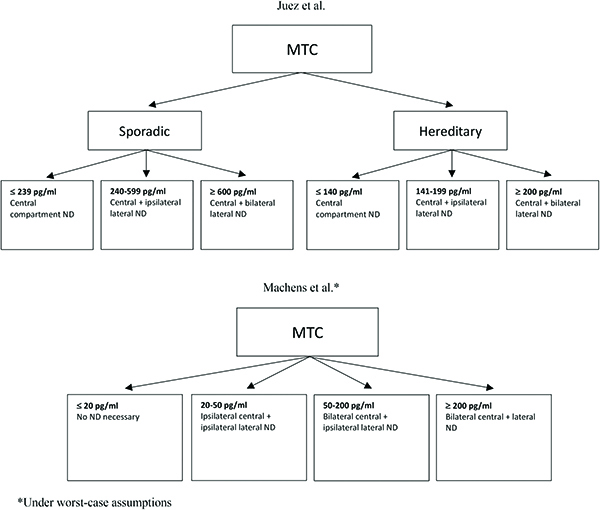
Presently, the American Thyroid Association and other authors recommend total thyroidectomy and central ND for the treatment of sporadic MTC. While calcitonin cutoffs for prophylactic lateral ND vary by guideline and study (Fig. 1), there is no consensus on whether prophylactic ND correlates with long-term survival. Based on currently available studies, not enough evidence exists to support the use of calcitonin alone as a predictor of the presence of post-operative neck lymph nodes. Rather, patients with the above-published calcitonin levels should undergo stronger consideration for more extensive ND, but the calcitonin level should be considered alongside pre-operative imaging and other clinical factors.