INTRODUCTION
Tracheoesophageal fistula (TEF) without esophageal atresia, also termed H-type, N-type, Gross type E, or isolated fistula, can be congenital or acquired. Children with H-type TEF typically present with cough during feeding, cyanotic spells, and recurrent pneumonia. Endoscopic repair of H-type TEF via bronchoscopy has traditionally been limited to long, narrow (<2 mm), recurrent TEFs, which often require multiple procedures with interposed material (i.e., fibrin glue) and the occasional addition of ancillary procedures such as an esophageal balloon or a biosynthetic mesh plug (J Pediatr Surg. 2008;43:238-245. Curr Opin Otolaryngol Head Neck Surg. 2016;24:510-515). Wide (>2 mm), short TEFs are notoriously difficult to repair endoscopically and have traditionally required a thoracoscopic or open approach (Curr Opin Otolaryngol Head Neck Surg. 2016;24:510-515).
Explore This Issue
July 2024We recently described suspending the esophagus with a laryngoscope to remove an intraluminal esophageal metal barbecue brush bristle in a child (Laryngoscope. 2021;131:E2066-E8). In that patient, the use of two hands under magnification with a wide field of view allowed the removal of a foreign body that would not have been accessible using a single instrument down a rigid esophagoscope. To our knowledge, suspension of the esophagus and the use of a microscope for endoscopic suture closure of a wide, short TEF have not previously been described. We report a patient for whom suspension microesophagoscopy was performed and describe how this approach allowed for improved management.
METHODS
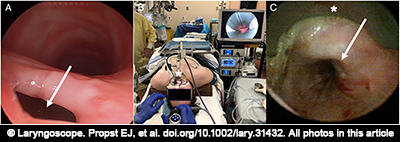
Figure 1. (A) Bronchoscopy demonstrating large, short tracheoesophageal fistula (TEF) (arrow). (B) Suspension esophagoscopy setup using Weerda distending laryngoscope (*). (C) Endoscopic view of esophagus in suspension with Weerda laryngoscope (*) showing exposure of TEF (arrow).
A 15-year-old male with prior Gross type C TEF repair, short stature, scoliosis, subaortic stenosis resection, ventricular septal defect repair, gastroesophageal reflux, and asthma was intubated due to parainfluenza A pneumonia and rhabdomyolysis. After five weeks of ventilation with a cuffed endotracheal tube, a tracheostomy was performed, with insertion of a size 6 Shiley DCT (cuffed with inner cannula). He was decannulated, but persistent aspiration pneumonia prompted flexible fiberoptic nasolaryngoscopy, which revealed a left vocal cord paralysis. Rigid bronchoscopy revealed an A-frame tracheal deformity and a large (4-mm diameter), short TEF just distal to it in the lower half of the trachea, likely in the location of the previous TEF repair (Fig. 1 ). This was a defect in the common party wall rather than a tract. The patient was referred to otolaryngology because he and his parents did not want to undergo open TEF repair, and it was felt that another long general anesthetic would not be well tolerated given his medical status. After discussing the very low likelihood that traditional transtracheal endoscopic methods (i.e., cautery and Tisseel) could close the large TEF, and that his rapid desaturations and narrow trachea would not allow suture closure from the tracheal side, the possibility of experimental suspension esophagoscopy and endoscopic suture repair was offered, and the family consented to the procedure.