INTRODUCTION
Bilateral vocal fold immobility can occur after iatrogenic injury, resulting in ankylosis of the cricoarytenoid joints, or can occur secondary to central nervous system insults, idiopathic and iatrogenic paralysis of the recurrent laryngeal nerves, or autoimmune disease. This often leaves patients with an untenable airway and may require a tracheostomy to bypass the upper airway obstruction.
Explore This Issue
March 2024Over the past several decades, there have been multiple attempts at surgical interventions to allow for breathing without the need for tracheostomy, with good success. Early attempts employed open techniques, and while these approaches were generally successful, they carried the morbidity often associated with open airway procedures.
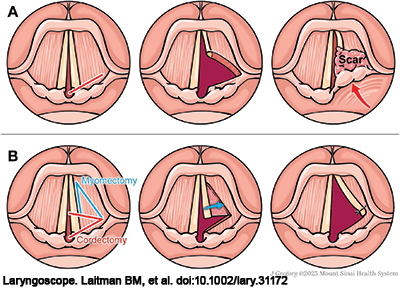
Figure 1. Traditional transverse cordotomy compared to TAM Cordotomy. (A) Traditionally, a transverse cordotomy is performed with an incision anterior to the vocal process taken laterally (left panel). While this can lead to initial release of the vocal fold and airway enlargement (middle panel), resultant granulation tissue and scarring can close this defect and bring the arytenoid forward once again, narrowing the airway (right panel). (B) In the TAM cordotomy, an additional anterior segment of muscle is resected (left panel) and the vocal fold mucosal flap is sutured laterally to the remaining lateral muscle border and false vocal fold (middle panel). This creates a triangular-shaped defect that is covered with mucosa, limiting restenosis (right panel).
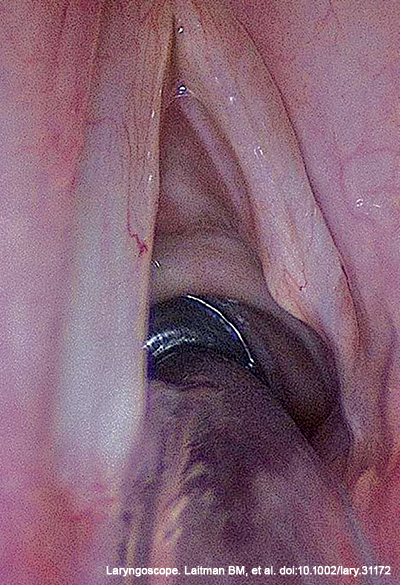
Bilateral vocal fold fixation or paralysis (BVCP) can leave patients with an untenable airway and may require a tracheostomy to bypass upper airway obstruction. To improve the airway obstruction or in an effort to decannulate patients after tracheostomy, treatment for bilateral vocal fold immobility necessitates lasting airway dilation. Currently, BVCP is often treated by transoral CO2 laser-assisted transverse cordotomy, but this procedure can lead to subsequent scarring at the wound bed resulting in re-narrowing of the airway and poor voice (Figure 1A).
Here, we propose a modification of the transverse cordotomy procedure that improves predictable airway and voice outcomes.
METHOD
We report on a variation of the transverse cordotomy that is meant to improve healing and provide mucosal coverage, which combines the transverse cordotomy (Ann Otol Rhinol Laryngol. 1991. doi:10.1177/000348949110000905) with a thyroarytenoid myectomy (Rev Paul Med. 1985. PMID:4035182) (TAM). This procedure has been performed on a series of patients over the past 10 years.