 Imaging of parathyroid adenomas, efficacy of functional rhinoplasty, an emerging therapy for recurrent respiratory papillomatosis, betahistine for Ménière’s disease, and the state of surgical training were all tackled by a panel of experts at the Triological Society Combined Sections Meeting in a series of Best Practice talks—condensed presentations on practical clinical considerations based on available evidence.
Imaging of parathyroid adenomas, efficacy of functional rhinoplasty, an emerging therapy for recurrent respiratory papillomatosis, betahistine for Ménière’s disease, and the state of surgical training were all tackled by a panel of experts at the Triological Society Combined Sections Meeting in a series of Best Practice talks—condensed presentations on practical clinical considerations based on available evidence.
Explore This Issue
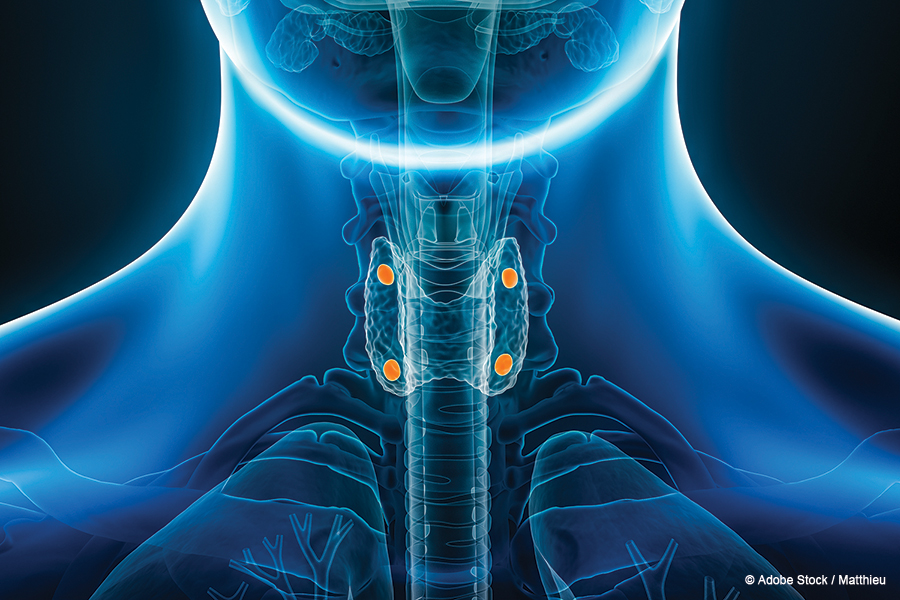
June 2024Parathyroid Adenoma Imaging
All of the most common imaging modalities for parathyroid adenomas have merit, depending on the situation and surgeon comfort, said Samir Khariwala, MD, MS, chair of otolaryngology–head and neck surgery at the University of Minnesota, Minneapolis, in one presentation.
Perhaps [MRI] is an adjunct—not necessarily superior, but a different modality—that can be used when the adenoma is not identified on sestamibi.” — Samir Khariwala, MD, MS
These parathyroid adenomas can be very difficult cases depending on the type. “As any surgeon who does this kind of procedure knows, localized [and] non-localized adenomas … require significantly different planning,” Dr. Khariwala said. “A localized adenoma is a really quick operation; a non-localized adenoma can be sometimes even soul-crushing.”
When parathyroid adenomas are identified accurately, the cost, the length of surgery, and the need for additional procedures are reduced, “so obviously we want to try to identify them as accurately as possible,” he said.
Several modalities are available for adenoma detection, and the one that’s chosen may vary by the surgeon and the patient.
One study evaluated magnetic resonance imaging (MRI) alone and as an adjunct to sestamibi scanning. Researchers found that MRI detected 16 of 25 adenomas, compared with 18 of 25 for sestamibi, but it also found four of seven that were not identified on sestamibi.
“So perhaps [MRI] is an adjunct—not necessarily superior, but a different modality—that can be used when the adenoma is not identified on sestamibi,” he said.
A 2016 paper on guidelines by the American Association of Endocrine Surgeons suggested that the imaging modality for adenomas should be chosen by the experienced surgeon, that ultrasound is the most cost-effective, and that MRI and venous sampling could be considered when there is a challenging component to the case, such as a re-do or a non-localized adenoma (JAMA Surg. 2016;151:959–968).
A meta-analysis including 43 studies found that ultrasound and sestamibi showed similar efficacy, and that 4D-computed tomography (CT), a newer modality, may be superior, but too few studies exist to make a conclusion, Dr. Khariwala said (Ann Surg Oncol. 2012;19:577–583).
Another study, in 2019, compared fine needle aspiration (FNA) with parathyroid hormone (PTH) washout to ultrasound and sestamibi and found that sensitivity, specificity, and positive and negative predictive values were all best for FNA