 A new study has put artificial intelligence (AI) to use to show that patients with non-flaccid facial paralysis express significantly more happiness following the removal of a facial muscle, according to findings presented at the 2024 Triological Society Combined Sections Meeting.
A new study has put artificial intelligence (AI) to use to show that patients with non-flaccid facial paralysis express significantly more happiness following the removal of a facial muscle, according to findings presented at the 2024 Triological Society Combined Sections Meeting.
Explore This Issue
June 2024The analysis gives clinicians data to help them counsel patients on outcomes to expect after depressor anguli oris (DAO) excision, said Samuel O’Rourke, BS, a medical student at the University of North Carolina (UNC) School of Medicine, Chapel Hill, who presented the findings and worked with Matthew Q. Miller, MD, director of the UNC Facial Nerve Center.
In non-flaccid facial paralysis, facial muscles still have neural input—unlike the less common flaccid facial paralysis—but the nerves are miswired, resulting in the facial muscles being out of balance. When patients smile, they often don’t express the happiness they’re feeling, but a negative emotion, Dr. Miller later told ENT Today.
“What we have really learned the past five to 10 years is that much of what drives a patient to treatment is the psychosocial aspect of facial paralysis, as much as it is the functional aspect,” said Dr. Miller. “What a lot of [patients] really, really hate is not being able to express themselves. When they want to smile, their smile doesn’t necessarily show happiness. It may show disgust, it may show discontent, it may show anger, it may show sadness.”
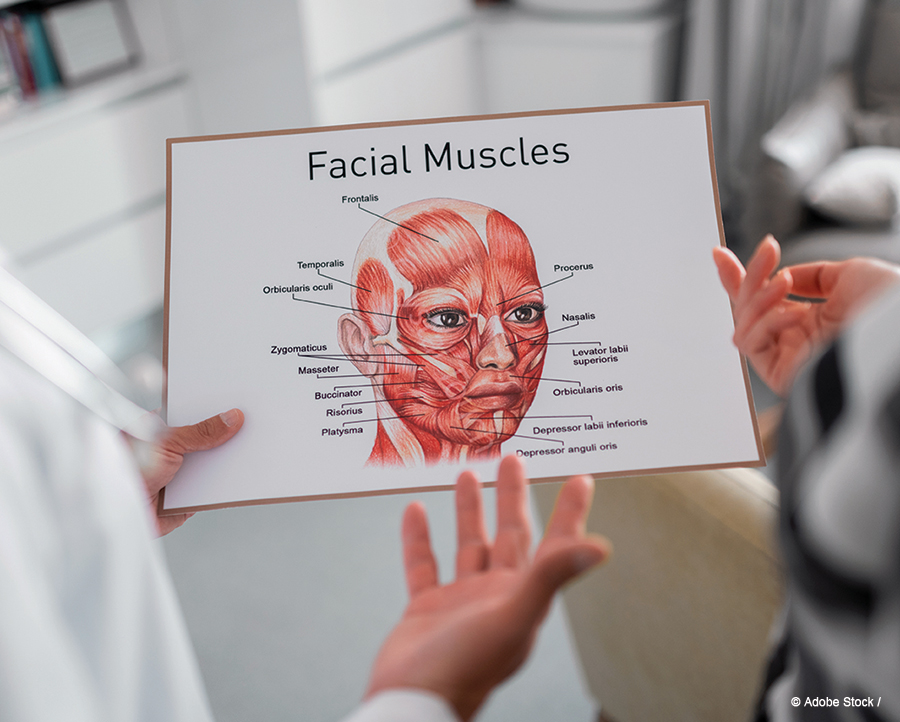
The DAO muscle, which brings the corner of the mouth down, essentially outcompetes the smile muscle as it tries to bring the corner of the mouth up, he said. Other than helping people frown, there is not much use for the DAO muscle, he said, and DAO excision was first introduced as a cosmetic procedure about 20 years ago to lift the corner of the mouth and soften the marionette lines in the face.
“It does help you frown, but I have yet to meet a patient who cares about frowning,” Dr. Miller said.
The procedure can be done in the clinic without general anesthesia in about 20–25 minutes, he said. It can be done through the mouth, without scarring.
Studies have already found that, after DAO excision, clinicians think the smile is better, patients think the smile is better, and patients show more teeth, have an improved smile shape, and have a bigger smile. What hadn’t been studied is how observers perceive emotions expressed by patients when smiling and whether these emotions change after surgery.
Dr. Miller said that layperson studies can be difficult to do because they’re time-consuming and some patients don’t like to have random people observing and evaluating them. The use of AI avoids those hurdles.
The software employed in Dr. Miller’s research uses deep neural networks trained on thousands of photos to assign emotions to a given photo or video clip. It was developed for marketing purposes to analyze consumer behavior but is increasingly being used in medical research.
In the study, which used video clips of patients smiling, the 68 participants were found to express 11% more happiness when they smiled (P<0.05) after surgery—from 40% happiness before DAO excision to 51% afterward. Previous studies have found that people without facial paralysis express about 68% happiness when they smile.
“We’re still not back to where the controls are at 68%, but we’re closer—we’re actually significantly closer,” Dr. Miller said. Patients notice the improvement. He thinks this increased ability to express happiness is one of the reasons over 90% of patients are happy they have had DAO excision and would choose to undergo the procedure again when asked a month after surgery.
Dr. Miller said the study’s findings can improve conversations with patients.
“It helps me counsel patients and give them a better idea of expected outcomes as I’m talking to them in the clinic. Quality data improve patient counseling and outcome research, both of which help us provide better care to patients,” he said. “I think the 11% is less important than just me being able to say, ‘We know most people look happier when they smile after surgery.’ That’s what a patient wants to hear.”
Thomas R. Collins is a freelance medical writer based in Florida.