INTRODUCTION
Failure to obtain tumor-free surgical margins as well as poor communication across departments contribute to worse surgical outcomes (Vignettes in Patient Safety (pp. Ch. 1). IntechOpen; 2018. doi: 10.5772/intechopen.78014; Am J Surg. 1976 doi: 10.1016/0002-9610(76)90314-7). This is especially true in head and neck surgery, where upper aerodigestive tract oncologic surgeries have high rates of positive margins (Sci Rep. 2018. doi: 10.1038/s41598-018-23403-5). Leaving positive margins unaddressed requires additional treatment, increasing cost, and burden to the patient and healthcare system (Sci Rep. 2018. doi: 10.1038/s41598-018-23403-5).
Explore This Issue
December 2023Several methods have been proposed to lower the rate of positive surgical margins by improving intraoperative communication. We previously demonstrated the effectiveness of rendering virtual models of head and neck resection specimens (Head Neck. 2023. doi: 10.1002/hed.27171), and we are currently demonstrating the utility of 3D surgical defect models (under review).
However, while these innovations improved communication from the frozen section laboratory to the operating room, visual communication from the operating room to the frozen section laboratory has not yet evolved. Currently, there is no accepted standard for intraoperative documentation of the location and breadth of supplemental margins harvested.
Here, we demonstrate that using Procreate, an iPad-based digital illustration software, to annotate resection specimen models and surgical defects improves efficiency and legibility of annotation. This method establishes a bidirectional exchange of visual information between surgeon and pathologist—specifically during supplemental margin analysis—and enables more accurate documentation of margins at risk.
METHOD
The Procreate application was utilized on iPad Pro (4th generation) to intraoperatively annotate 3D renderings of head and neck surgical defects and resection specimens at Mount Sinai West Hospital, New York, N.Y. As we demonstrated previously, a handheld 3D scanner was used immediately following resection to capture the complexities of the surgical defect and render a virtual 3D model (Head Neck. 2023. doi: 10.1002/hed.27171).
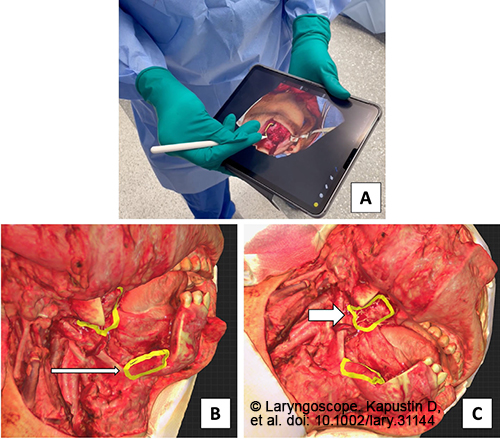
Figure 1. Intraoperative surgical defect annotation. (A) Surgeon maintains sterility in the operating room while drawing the location and breadth of supplemental margins harvested on the 3D defect scan. (B and C) Annotated defect scan for a composite oral cavity resection included a segmental mandibulectomy and floor of mouth resection. Annotations indicate supplemental margins taken medial to the retromolar trigone (short arrow, C) and the right mylohyoid margin (long arrow, B).
Additionally, following removal of the specimen, a 3D rendering of the resection specimen was generated using a SHINING 3D scanner and companion software as detailed in Saturno et al. (Head Neck. 2023. doi: 10.1002/hed.27171). After rendering the 3D model, the specimen was processed to assess margins.
To preserve the 3D model’s coloring, the open-source graphics software Blender was used to merge the 3D file (OBJ) with its color/texture files (JPEG/MTL). The new file was then exported to the iPad and imported into Procreate where touchscreen manipulation enabled the use of 3D rotation. Intraoperatively, an over glove was worn to maintain sterility, and the surgeon drew on the 3D model of the surgical defect using a stylus. The surgeon indicated the precise location and breadth of each supplemental margin—in other words, the additional tissue harvested for the purpose of addressing a previously positive or close margin.