 TRIO Best Practice articles are brief, structured reviews designed to provide the busy clinician with a handy outline and reference for day-to-day clinical decision making. The ENTtoday summaries below include the Background and Best Practice sections of the original article. To view the complete Laryngoscope articles free of charge, visit Laryngoscope.com.
TRIO Best Practice articles are brief, structured reviews designed to provide the busy clinician with a handy outline and reference for day-to-day clinical decision making. The ENTtoday summaries below include the Background and Best Practice sections of the original article. To view the complete Laryngoscope articles free of charge, visit Laryngoscope.com.
Explore This Issue
June 2023BACKGROUND
Paragangliomas are uncommon tumors of the head and neck that contain membrane-bound somatostatin type 2 receptors (SSTR-2), making them easy to detect with radiolabeled peptide receptor imaging. Some of these tumors may present in a typical fashion and can be identified with conventional imaging such as computerized tomography or magnetic resonance imaging (MRI). There are classic signs associated with head and neck paragangliomas seen on standard imaging such as the “lyre sign,” in which the internal and external carotid arteries are splayed or a vascular mass on the promontory of the middle ear. A “salt and pepper” appearance on contrast MRI T1-weighted images is also strongly suggestive of paraganglioma.
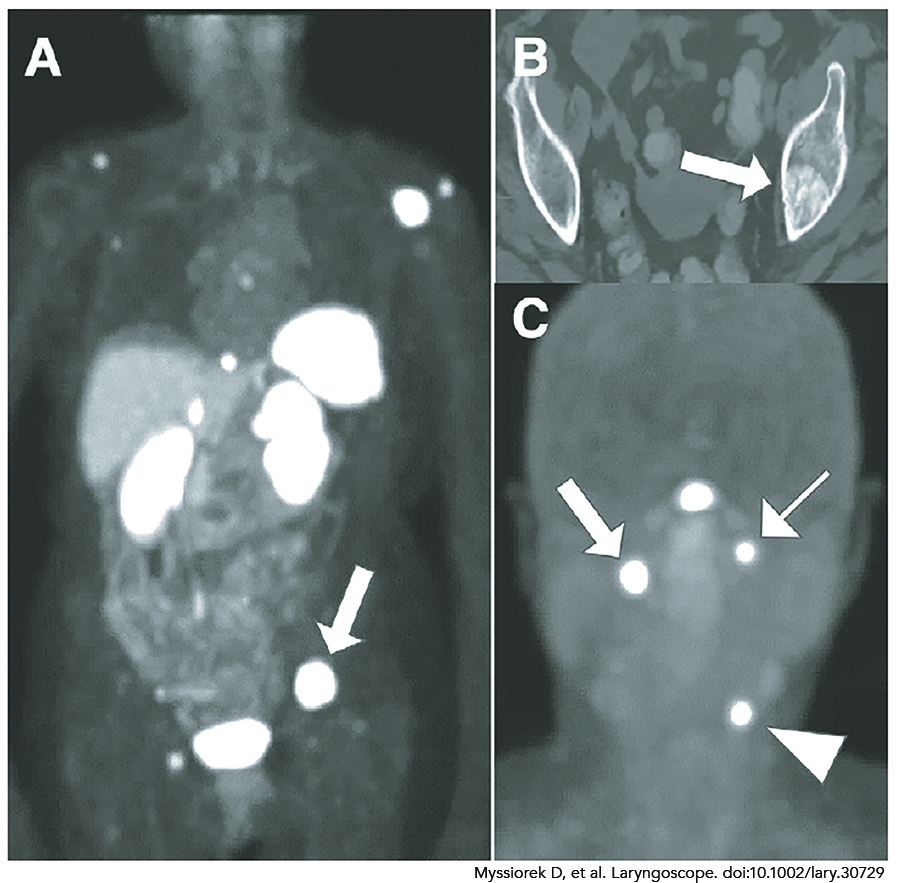
Figure 1. An 81-year-old female with prior resection of left infratemporal paraganglioma. Head and neck images showed no local recurrence, but small bone metastases were present. (A) On 68Ga-Dotatate PET, normal activity is seen in the liver, spleen, right adrenal, kidneys, bowel, and bladder. All other areas of activity were confirmed bone metastases. Arrow shows lesion seen on CT (B). (B) Sclerotic metastasis. (C) 54-year-old female with previously treated pheochromocytoma. On 68Ga-Dotatate PET, there is intense uptake in a right vagal paraganglioma (arrow), a left jugular paraganglioma (thin arrow), and in a left carotid paraganglioma (arrowhead). Central activity represents normal uptake by the pituitary.
There are other situations where nuclear medicine imaging will be an important tool in the head and neck surgeon’s arsenal. Paragangliomas can be multifocal, familial, recurrent, and metastatic. All of these can be evaluated via nuclear medicine, taking advantage of the SSTR-2 receptors and their affinity for radiolabeled somatostatin analogs (Laryngoscope. 2005;115:1707–1716).
Treatment planning for multiple or recurrent paragangliomas can be challenging and knowledge of the location of all paraganglioma tissue is critical. Familial paraganglioma syndrome patients are at high risk for early onset and multifocality. If a person is suspected to harbor a familial tumor (family member with paraganglioma, vagal paraganglioma, early age at detection, and multiple sites) ruling out other sites of paraganglionic tissue is necessary. The succinate dehydrogenase subunit B (SDHB) variant of familial paraganglioma syndrome is associated with a higher degree of malignancy. If a genetic pedigree is determined to be SDHB, nuclear medicine imaging looking for multiple tumors and metastases (Figure 1A, 1B) is highly recommended.
BEST PRACTICE
Nuclear medical imaging is strongly recommended in the diagnosis of paragangliomas that are familial, SDHB variants, malignant, or potentially multifocal. Paragangliomas that have classic presentations such as sporadic carotid paragangliomas or tympanic paragangliomas do not routinely require peptide receptor imaging. The uncommon nature of these tumors would make large prospective studies difficult to perform.
