Introduction
Pediatric tracheobronchial foreign body aspiration (FBA) is a common and potentially life-threatening event. Children under 3 years of age account for 77% of pediatric visits to the emergency department for aspiration, with food items being the culprit in 69% of cases (MMWR Morb Mortal Wkly Rep. 2002;51:945-948). Approximately 4% of patients admitted with FBA suffer anoxic brain injury or death (Laryngoscope. 2015;125:1221-1224). Missed or retained airway foreign bodies can cause pneumonia, lung abscess, bronchiectasis, or atelectasis.
Explore This Issue
December 2021The challenge of guiding a rigid linear instrument through a nonlinear path behooves surgeons to create innovative strategies for foreign body removal.
All children with suspected FBA require tracheobronchial examination for diagnosis and management (Pediatr Rev. 2000;21:86-90). The presence of a foreign body can be confirmed using flexible or rigid bronchoscopy or computed tomography scan if the patient is stable and old enough to not require general anesthesia. If identified, an airway foreign body requires immediate removal. Rigid bronchoscopy is commonly used for foreign body removal as it allows ventilation, visualization, instrumentation, airway control, and hemorrhage control, particularly important in children due to their narrower airways (Am J Respir Crit Care Med. 2015;191:1066-1080). Reaching a small foreign body in certain branches of the distal airway in small, young children may not be possible, however, due to limitations in instrument caliber and angulation. Flexible suction catheters, Fogarty balloons, and urological wire baskets are all options to access these smaller airways but are limited to the straight line of attack offered by the rigid bronchoscope. The challenge of guiding a rigid linear instrument through a nonlinear path behooves surgeons to create innovative strategies for foreign body removal. We describe a novel technique for pediatric distal airway foreign body removal using a bent flexible suction catheter to guide a urological wire basket during rigid bronchoscopy.
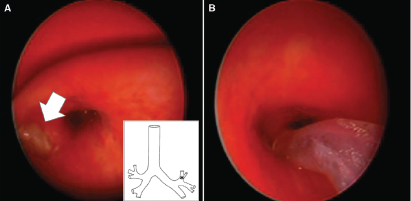
Figure 1. Bronchoscopic view during foreign body removal. (A) Peanut fragment seen lodged into the superior division of the left superior lobar bronchus (Inset *). (B) A 6-Fr flexible suction catheter with the tip bent was used to access the foreign body.
Gabinet-Equihua A, et al. Laryngoscope. doi:10.1002/lary.29523
Method
A 3-year-old boy presented to the emergency department with wheezing and dyspnea several hours after a witnessed choking episode involving peanuts. Chest X-ray inspiratory and expiratory views did not demonstrate an airway foreign body or air trapping. He was admitted to the hospital and underwent urgent rigid bronchoscopy later that day due to worsening oxygenation.
The patient was placed under general anesthesia, with spontaneous ventilation maintained using intravenous midazolam, propofol, remifentanil, and dexmedetomidine as well as topical lidocaine to the glottis. A 30-cm, 4.0 rigid bronchoscope with a 30-cm × 2.9-mm telescope was used to identify and remove multiple peanut fragments in both main bronchi. Additional fragments in the right lower, right upper, and left lower bronchi were also identified and removed. A 36-cm × 2.9-mm telescope was placed through the 30-cm, 4.0 rigid bronchoscope, and a final fragment in the superior division of the left superior lobar bronchus was identified (Figure 1). Multiple removal attempts using optical peanut forceps, rigid suction, and 4-Fr and 6-Fr flexible suction catheters were unsuccessful. Neither a Fogarty balloon nor a urological wire basket could be angled appropriately to enter the bronchus and reach the fragment. We therefore bent a 6-Fr flexible suction catheter, which allowed us to approach the foreign body (Figure 2). The peanut fragment, however, was wedged too tightly to remove it with suction or to advance the catheter distally to flush it out with saline. A 2.2-Fr urological wire basket was able to pass through the 6-Fr suction catheter, and both were advanced down the side port of the 4.0 rigid bronchoscope with a 2.9-mm telescope in place. The bend in the catheter allowed the basket to be guided to the site of obstruction and subsequently slipped beyond the peanut fragment (see the supporting video). The fragment was then ensnared and removed. The patient maintained good oxygenation throughout the procedure, and no other foreign bodies were identified. He was observed overnight with continuous monitoring and discharged home the following day. Institutional research ethics board approval was waived for this case report.