© Mark_Kostich / shutterstock.com
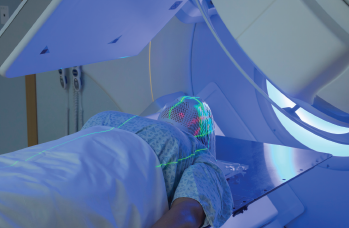
HPV-driven oropharyngeal cancers respond better to radiotherapy than other treatments. However, despite this and other benefits, radiation therapy has a host of drawbacks, including long-term side effects and even treatment-related morbidity in some cases. Given these disadvantages, debates continue regarding whether or not radiotherapy is the right way to treat these patients.
Explore This Issue
November 2019On the positive side, radiation combined with chemotherapy results in high cure rates: 85% of patients with locally advanced disease live five years or longer (Lancet. 2019;393:40–50). For lower stages of HPV-driven oropharyngeal cancer, the survival rate is even higher, and only radiation (no chemotherapy) is required. Radiotherapy is also non-invasive and doesn’t require anesthesia. “Because of these benefits, radiation can be given to the vast majority of patients, even those with other significant medical problems,” said Stephen Ramey, MD, assistant professor of radiation oncology at Augusta University in Georgia.
David Clump, MD, PhD, assistant professor in the department of radiation oncology at the University of Pittsburgh Medical Center Hillman Cancer Center, said that HPV+ small volume oropharyngeal squamous cell carcinomas have a failure rate of less than 10% when treated with radiation therapy delivered over six weeks (Int J Radiat Oncol Biol Phys. 2010;76:1333–1338). For patients with more advanced disease, cytotoxic chemotherapy is combined with radiation to improve cure rates.
Although early T-stage oropharyngeal cancers can also be treated surgically, these procedures may be followed by adjuvant radiation, with or without chemotherapy, depending on pathologic features, said Ken Byrd, MD, associate professor of head and neck surgery at Augusta University.
Disadvantages of Radiotherapy
On the negative side, patients who undergo radiation treatment must often endure fatigue, skin erythema and breakdown, dysphagia due to inflammation of tissues, mucositis, pain, loss of taste, lymphedema, and a higher risk of depression. In the long term, these patients have risks of fibrosis and decreased range of motion of the neck, along with xerostomia and dental caries. “Fibrosis of pharyngeal and cricopharyngeal musculature can lead to longer term swallowing difficulties and risk of aspiration pneumonia,” said Brandi R. Page, MD, assistant professor of radiation oncology and molecular sciences, and assistant professor of otolaryngology, Johns Hopkins School of Medicine in Baltimore. “Severe toxicities such as osteoradionecrosis or fistula are possible.”
When patients receive both chemotherapy and radiation treatment, mucositis is a common acute toxicity. Mucositis persists and results in pain, dysphagia, and weight loss. It requires the use of gastrostomy tubes and narcotics to combat the pain. Patients also suffer from sequelae such as fatigue, nausea, emesis, nephrotoxicity, and ototoxicity. “Such acute toxicities can require breaks in treatment, which can lead to suboptimal treatment efficacy,” said Cherie-Ann O. Nathan, MD, professor and chair of the department of otolaryngology/head and neck surgery at Louisiana State University Health Sciences Center and director of head and neck surgical oncology at Feist-Weiller Cancer Center, both in Shreveport, La.
Patients with HPV+ oropharynx cancers are often in their 40s and 50s, so long-term toxicities can impact them for decades. Furthermore, the percentage of patients living after treatment is increasing because these patients are often younger and healthier than previous patient cohorts.