What is the cumulative effect of diagnostic steps for primary tumor identification in patients with head and neck squamous cell carcinoma of unknown primary (HNSCCUP)?
Bottom Line: A stepwise approach to primary tumor identification identifies a primary tumor in a majority of patients.
Explore This Issue
July 2019Background: After an initial history and physical examination, and determining the metastasis’ HPV status, HNSCCUP evaluation aims at primary tumor identification. This begins with diagnostic imaging (CT, MRI, and/or fluorodeoxyglucose-positron emission tomography [FDG-PET]/CT), then ipsilateral palatine tonsillectomy if needed, then bilateral palatine tonsillectomy if needed. Although the effectiveness of each has been evaluated individually, there is a lack of data on their cumulative effect applied in sequence.
Study design: Retrospective analysis of 110 patients diagnosed with HNSCCUP between 2003 and 2015.
Setting: Johns Hopkins Bloomberg School of Public Health, Baltimore.
Synopsis: All patients underwent direct laryngoscopy with biopsy of suspicious lesions, which identified a primary tumor in 34 patients. Forty-seven patients underwent palatine tonsillectomy, with 17 identified with primary tumors. Fourteen patients underwent subsequent TORS lingual tonsillectomy, and eight primary tumors were identified. FDG-PET/CT was used prior to operative diagnostic evaluation in 77 patients. Among these, 23 were suspicious for a primary site. Ten of the 23 had the primary tumor identified by direct laryngoscopy. Seven additional tonsillar primaries were identified by palatine tonsillectomy, yielding a cumulative identification of 17 of 23. Twenty-five of 54 primary tumors were cumulatively identified in patients with negative FDG-PET/CT. For 80 HPV-positive patients, 29 primary tumors were identified after direct laryngoscopy with biopsies. Thirty-four underwent palatine tonsillectomy; fifteen of these revealed the primary tumor. Eleven underwent TORS lingual tonsillectomy, which identified eight new primaries. Patients with HPV-positive tumors had longer overall survival rates than patients with HPV-negative tumors. Limitations included the study’s retrospective nature, data from a single institution, nonrandom diagnostic evaluation and treatment variations, and outcomes that are not necessarily generalizable.
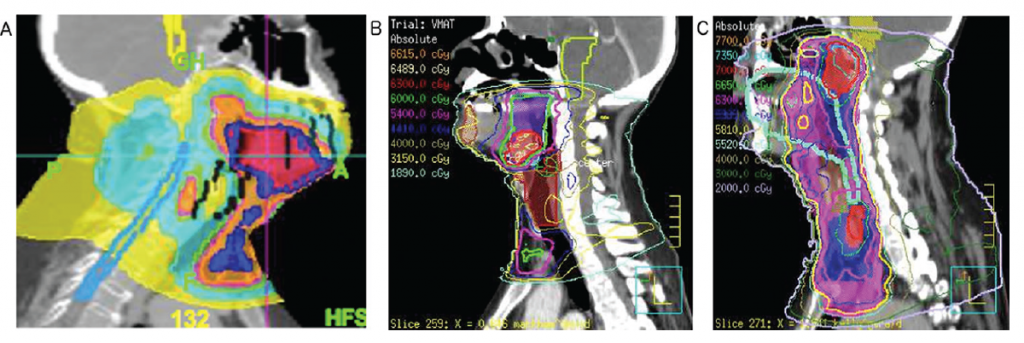
Images from treatment plans illustrating differences in radiation treatment for a patient with (A) an identified HPV-positive base-of-tongue primary tumor, (B) an HPV-positive metastasis without identified primary, and (C) an HPV-negative metastasis without identified primary.
© 2019 The American Laryngological, Rhinological and Otological Society, Inc.