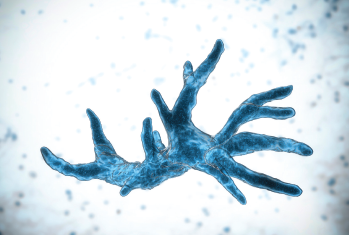
Balamuthia mandrillaris.
© Kateryna Kon / shutterstock.com
Recent news of a 69-year-old woman in Seattle who died of amoebic meningoencephalitis (AM) from the rare amoeba Balamuthia mandrillaris again reminds us of the need for physicians to counsel patients about the most appropriate and safest way to irrigate their sinuses. Although the source of the infection has not been proven, it is speculated that it came from the tap water she used in her neti pot for nasal irrigation (Int J Inf Dis. 2018;77:18-22).
Explore This Issue
February 2019Although the incidence of such a fatal brain infection from nasal irrigation is rare, with only three other cases of AM reported in the United States (all due to infection with the amoeba Naegleria fowleri) (Int Forum Allergy Rhinol. Published online ahead of print January 18, 2019. doi: 10.1002/alr.22294), the sheer possibility of such an event has generated considerable concern among patients and physicians and has led to guidelines by the Centers for Disease Control and Prevention (CDC) on safe ritual nasal rinsing (See “CDC Guidelines,” below).
These guidelines are not new to otolaryngologists but they may be unknown to patients or, if known, not followed. Education is key in getting patients to understand the need for safe routine nasal irrigation practices, particularly patients with chronic rhinusitis who require such irrigation. However, physicians also need to grapple with the reality that compliance with regular nasal irrigation may be compromised and chronic conditions worsened if patients feel that the burden of having to practice safe irrigation techniques requires too much effort.
Perspective Is Paramount
Given the strong reaction and concern that stories such as the Seattle fatality generate among patients, and the subsequent need for otolaryngologists to educate their patients about safe nasal irrigation in the context of rare infection and compliance issues, Timothy Smith, MD, MPH, professor and chief in the division of rhinology and sinus/skull base surgery in the department of otolaryngology-head and neck surgery at Oregon Health and Science University in Portland and a member of the ENTtoday editorial advisory board, urged otolaryngologists that perspective is paramount. “At what point do additional safety measures become more dangerous?” he questioned in a Letter to the Editor published in the International Forum of Allergy and Rhinology (Published online ahead of print January 18, 2019. doi: 10.1002/alr.22294).
He elaborated in an interview with ENTtoday: “While the recent death is very tragic, at what point do our recommendations to be as safe as possible to avoid an extremely rare infection actually create a situation where our patients will become noncompliant and be harmed by the noncompliance to their therapy?” he asked. “From a public health stand point, you can probably make the argument that more people will be harmed trying to following somewhat burdensome recommendations than are going to be harmed by a rare amoeba infection.”
In the published letter, Dr. Smith interviewed four other otolaryngologists on their thoughts regarding water sources for nasal irrigation. As a whole, he said, they all agreed that the safest irrigation water source is either distilled water or boiled water that has cooled. However, he also emphasized the shared concern to educate patients on how to weigh the rare risk of infections with noncompliance to the CDC recommendations of appropriate water sources for nasal irrigation. “We need to have a conversation with patients about the risks of an exceedingly rare but deadly infection versus the risk of noncompliance of their therapy,” he said. “There is probably room for shared decision making here.”
That said, Dr. Smith emphasized the importance of certain populations following the CDC guidelines. These include immunocompromised people, people who use well water, and people who are concerned with their water quality.