SCOTTSDALE—A wide array of new research was presented at the Triological Society Combined Sections Meeting, held January 18–20 of this year, covering topics ranging from new procedures to the state of otolaryngology research to attempts to perfect the use of gum in cancer prevention.
Explore This Issue
May 2018Pre-Op Evaluations in Pediatric Airway Reconstructions Could Use Improvement
The Paul H. Holinger, MD, Resident Research Award went to University of Cincinnati researchers who looked at optimal preoperative evaluation of pediatric airway reconstruction patients. They reviewed records for all patients undergoing the procedure at the center in 2013, evaluating whether or not all components of the pre-op evaluation were completed, including screening for oxacillin-resistant Staphylococcus aureus (ORSA), impedance testing, aspiration risk assessment, flexible bronchoscopy, microlaryngoscopy and bronchoscopy, and esophagogastroduodenoscopy. Douglas Von Allmen, MD, a resident at the University of Cincinnati, reported that all of the components of the review had been completed in fewer than half of the cases—just 26 of the 65 charts reviewed. More research is needed to ascertain the impact on outcomes, he said.
Study Identifies Gaps in Otolaryngology Patient Safety Research

Single-stage laryngotracheal reconstruction
© Int Arch Otorhinolaryngol / National Library of MedicinE
The Henry Williams, MD, Resident Research Award went to a systematic review assessing patient safety and quality improvement research in otolaryngology-head and neck surgery. Researchers examined the Ovid MEDLINE, Cochrane, PubMed, and Google Scholar databases. The findings, presented by John Gettelfinger, MD, a resident at Indiana University in Indianapolis, showed that the most common subspecialties examined were head and neck and pediatric otolaryngology, most commonly focusing on complications or risk factors and residency and education. “Knowledge gaps for future research include dedicated facial plastic surgery and laryngology patient safety/quality improvement, equitable care studies, and the World Health Organization category of studies translating evidence into safer care,” researchers wrote.
Researchers Assess Bronchiectasis in LTE Clefts
The Lawrence R. Boies MD, Resident Research Award went to researchers at the University of Cincinnati who studied the rates of bronchiectasis on CT, and its relationship to swallowing dysfunction, measured by video swallowing study or endoscopic exam, among patients with laryngotracheoesophageal (LTE) clefts.
The investigators conducted a retrospective chart review of children who underwent repair for LTE clefts between 2000 and 2013, with 91 patients included. Those with a deep notch, Type I, or Type II clefts were considered low-grade clefts, and Type III clefts were considered high-grade.
In findings presented by resident David Lee, MD, the study concluded that 32% of patients had bronchiectasis and 63% demonstrated aspiration or penetration, with no significant differences in rates of either bronchiectasis or aspiration/penetration for those with low-grade versus high-grade clefts. “Both CT findings and swallowing studies are important to evaluate aspiration in LTE cleft patients,” they said.
‘Lean’ Method Improves Complication Rates
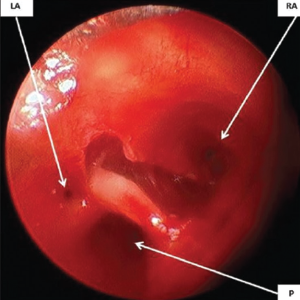
Rigid bronchoscopic view of the laryngotracheo-oesophageal cleft showing three openings: Right anterior (RA), left anterior (LA) and posterior (P).
© BIndian J Anaesth / National Library of Medicine