What are the clinical presentation and the role of the otolaryngologist in evaluating eosinophilic esophagitis (EoE) at a tertiary pediatric hospital?
Bottom line
Patients with EoE frequently present to otolaryngology undiagnosed in the first five years of life, making esophagoscopy with biopsy an important adjunct to airway endoscopy in children with refractory aerodigestive symptoms.
Explore This Issue
June 2017Background: EoE diagnosis requires esophageal dysfunction symptoms, esophageal eosinophilia on esophageal biopsy, and exclusion of alternative causes of esophageal eosinophlia. Recently, there has been increased recognition of EoE as a cause of gastrointestinal morbidity and reduced quality of life in affected children, as well as EoE airway manifestations being a possible cause of recurrent croup, stridor, dysphonia, and chronic cough. As a consequence, the otolaryngologist’s role is evolving.
Study design: Retrospective review of 251 pediatric patients with an EoE diagnosis from 2003 to 2015.
Setting: Children’s Hospital of Pittsburgh, Pa.
Synopsis: Overall, 26% of patients presented initially with airway symptoms including chronic cough, dysphonia, stridor, or recurrent croup. Ninety-seven percent of patients had GI symptoms on presentation, the most common being dysphagia, recurrent emesis/nausea, and abdominal pain, or food regurgitation. Departmental sites of initial patient presentation were: gastroenterology 67%, otolaryngology 18%, allergy/immunology 3%, and emergency department 13%. Of patients initially evaluated by otolaryngology, 82% were diagnosed with eosphageal eosinophilia during diagnostic panendoscopy, while 18% were later diagnosed by the GI service. Median time to diagnosis did not depend on initial presentation site. Patients initially presenting to otolaryngology were significantly younger than those presenting to GI, and airway symptomatology was more common.
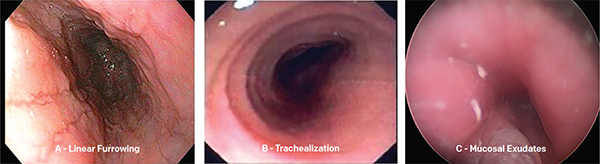
Common endoscopic abnormalities seen in patients with eosinophilic esophagitis.
Credit: Copyright 2017 The American Laryngological, Rhinological and Otological Society, Inc.
Endoscopic esophagus appearance was normal in 17% of patients with pathologically confirmed esophageal esosinophilia; linear furrowing was the most common abnormality noted. Airway endoscopy was performed in 25% of the otolaryngology cohort; common findings included tracheal cobblestoning, laryngomalacia, and subglottic stenosis.
Ultimately, 14% of patients were diagnosed by otolaryngology on the basis of esophageal biopsy results during diagnostic panendoscopy. In only 18% of cases evaluated by otolaryngology was the diagnosis missed and subsequently made by GI.
Citation: Kubik M, Thottam P, Shaffer A, Choi S. The role of the otolaryngologist in the evaluation and diagnosis of eosinophilic esophagitis. Laryngoscope. 2017;127:1459–1464.