The most dreaded complication of parotidectomy is facial nerve injury which is fortunately rare. A less devastating consequence that occurs in some patients is a pre-auricular depression caused by the absence of the parotid gland. While the problem is cosmetic, patients may feel uncomfortable with their appearance.
Explore This Issue
August 2016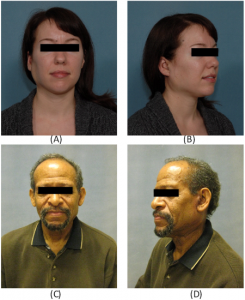
Two-week postoperative visit showing overcorrection of a right (A, B) and left (C, D) parotidectomy defect with free abdominal fat transfer reconstruction.
A number of surgical techniques to reconstruct this parotidectomy defect are available, including bipedicled sternocleidomastoid (SCM) muscle flaps, AlloDerm biomaterial, free tissue transfer, and free abdominal fat transfer (FAT). A recent study published in The Laryngoscope examines the use and effectiveness of the FAT transfer in reconstruction, including a realistic look at complication rates. The investigators say the procedure is technically simple and, when performed at the time of parotidectomy, improves facial symmetry and achieves excellent postoperative cosmetic results. (Laryngoscope [published online ahead of print May 30, 2016]. doi: 10.1002/lary.26025).
FAT Graft Procedure
In the study, 105 patients underwent 108 parotidectomies with FAT reconstruction between 2007 and 2015. The majority of patients had benign pathology and tumors that were smaller than 3 cm. Superficial parotidectomy was performed in 62 patients, and concurrent elective neck dissection was performed in eight patients.
During the FAT procedure, according to corresponding author Christine Gourin, MD, professor of otolaryngology in the department of otolaryngology-head and neck surgery at Johns Hopkins School of Medicine in Baltimore, a large piece of fat, along with some connective tissue, is removed from the abdominal area. “Rather than using a large incision, I prefer a pariumbilical incision,” said Dr. Gourin. “Not only are patients generally happier with the

Postoperative results six months after free abdominal fat transfer following right (A, B) and left (C, D) parotidectomy.
Credit: © 2016 The American Laryngological, Rhinological and Otological Society, Inc.
appearance, as the incision is cosmetically hidden, but a large incision in the area can mimic an appendectomy scar. That could be catastrophic if emergency medicine surgeons saw the scar and made an assumption that the patient had had other abdominal surgery, leading to a misdiagnosis of abdominal pain.”
One primary complaint about using standard fat grafts for parotidectomy defect reconstruction has been fat reabsorption and liquefaction. Although this may be a concern for fat harvested through liposuction methods, as well as for AlloDerm, which does not work well for filling substantial gaps, Dr. Gourin said that the connective tissue acts as an anchor to keep the transplanted fat in place. “Generally, the surgeon would take 30% more abdominal fat than what’s needed to repair the defect because despite the connecting tissue acting as an anchor, some reabsorption will happen, but with a large piece there is a better chance of the tissue surviving in its new location,” she added.
Only perhaps half of parotid surgeons perform [the FAT procedure], and I think its use depends to some extent on the age of the surgeon and where he or she trained. It wasn’t something I learned to do in my training; many of us just weren’t exposed to techniques for parotid defect reconstruction. —Christine Gourin, MD
Advantages, Disadvantages, and Complications
Although FAT grafts are a viable option for parotidectomy defect reconstruction, Dr. Gourin was surprised at the abdominal complication rate, with hematoma in eight patients and seroma in three patients. “The abdominal complication rate of 10% was a little higher than I thought it would be, but it really is the result of taking a large fat graft through a small incision,” she said. “But it’s a pretty realistic rate of donor site complications, and it’s important to report those honest data.”