MIAMI BEACH—Managing head and neck cancer involves high-stakes decisions that are full of nuance, with a need to weigh factors that range from a patient’s history to co-morbidities to tumor grade and location. Through the presentation of two clinical scenarios, a panel of experts dug into the details of case management of head and neck carcinoma during the Triological Society Combined Sections Meeting, held January 22–24 in Miami Beach, Fla.
Explore This Issue
April 2016Case 1: Left Parotid Tail Mass
A 38-year-old white female with a new-onset, 2-cm, left parotid tail mass has a history of Hodgkin’s lymphoma, for which she has undergone five courses of R-CHOP chemotherapy.
Francisco Civantos, MD, co-director of the division of head and neck surgery/otolaryngology at the University of Miami’s Sylvester Comprehensive Cancer Center in Florida, asked whether there was anything remarkable in her clinical exam. Panel moderator and case presenter Dennis Kraus, MD, director of the Center for Head and Neck Oncology at the New York Head and Neck Institute, said the patient reported that she generally felt pretty well.
Prior treatment of the head and neck might influence the effectiveness of future postoperative radiation.
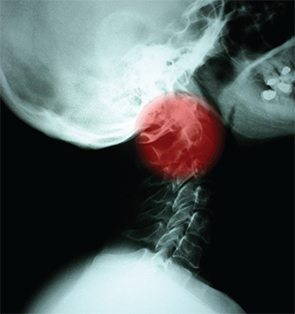
m.jrn/shutterstock.com
Richard Smith, MD, professor and vice chair of otorhinolaryngology-head and neck surgery and professor of pathology at Albert Einstein College of Medicine in New York City, said that recurrent lymphoma was possible. But Dr. Kraus said there were no obvious signs of that; on MRI, for instance, the mass appeared to be isolated, without infiltrating surrounding tissue. The mass was removed, Dr. Kraus said, and pathology found that the mass was a low-grade acinic cell carcinoma.
Maie St. John, MD, PhD, chair of head and neck surgery at the University of California, Los Angeles, and co-director of the UCLA Head and Neck Cancer, said the best course would probably be no further treatment. “At this point, if it’s well-encapsulated and low-grade, I would not offer neck dissection, but I would offer close surveillance,” she said. If there were no aggressive features, she would not offer postoperative radiation, she added.
Jonas Johnson, MD, professor and chair of the department of otolaryngology at the University of Pittsburgh School of Medicine, noted the importance of considering how close the mass is to the facial nerve, but Dr. Kraus said that was not a concern, given what was seen during surgery.
Ultimately, the tumor board opted for no more treatment. But high-grade acinic cell carcinomas might need a different response, Dr. Kraus said. “If you look at the literature for acinic cell, there is some controversy about our ability to grade them, although there’s clearly a distinction between low- and high-grade tumors,” he added. “There are reported cases, particularly in the higher grades, that some of these patients can develop metastatic disease.”
Case 2: Neck Node
A 68-year-old Hispanic male who, three years prior, received chemoradiation therapy for a T3N0 thoracic esophageal squamous cell carcinoma, now presents with a 3.5-cm left level 2 neck node. A needle biopsy, the pathologist determines, is HPV-negative metastatic squamous cell carcinoma that is negative for the p16(INK4a) tumor suppressor protein.