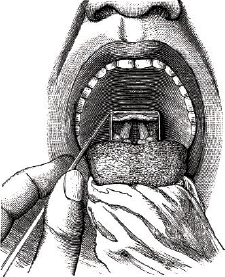
Image Credit: Morphart Creation/shutterstock.com
View of the vocal chords.
A group of experts on vocal fold paralysis tackled an array of patient cases, offering a window into their approaches during a session at the Triological Society 2015 Combined Sections Meeting.
Explore This Issue
April 2015The panel was chaired by James Netterville, MD, director of head and neck oncologic surgery at the Vanderbilt-Ingram Cancer Center in Nashville. Dr. Netterville teamed with panelists James Burns, MD, director of quality and safety for the Center for Laryngeal Surgery at Massachusetts General Hospital and associate professor of surgery at Harvard Medical School; Mark Courey, MD, medical director of the University of California San Francisco Voice Center; Gaelyn Garrett, MD, medical director of the Vanderbilt Voice Center; and Marshall Smith, MD, medical director of the Voice Disorders Center at the University of Utah in Salt Lake City.
Here are the cases and the panelists’ responses describing how each might approach care.
Case 1: Accidental Transection
A 33-year-old patient is taken to surgery for a total thyroidectomy, and a nonrecurrent laryngeal nerve is accidentally transected.
Dr. Courey said he would try to perform a primary repair of the nerve if a tension-free anastomosis was possible. Other than that, he said, he might try an ansa transfer. “I don’t know that I’d want to sacrifice the rest of the vagus nerve,” he said.
“If we could get end to end,” Dr. Netterville said, “then this might be a no brainer just to put this back together.”
Case 2: Cancer Affecting the Recurrent Laryngeal Nerve
In this case, a young woman has a total thyroidectomy with bilateral neck exploration with post-operative bilateral vocal cord paralysis. She then has an elective tracheotomy.
At six months, the left fold is functioning again, and the right is still paralyzed. Multiple positive nodes are found; papillary thyroid cancer is invading the recurrent laryngeal nerve (RLN). The nodes are removed. “There’s no ansa hypoglossi, there’s no ansa cervicalis, so we’re starting to limit our options for primary innervation,” Dr. Netterville said.
Dr. Smith said there were still avenues available. “There are some options with the vagus, with the branch to the thyrohyoid muscle, which drops down off the hypoglossal, which you can jump with an interposition graft,” he said.
The panelists talked about medialization because, if re-innervation is attempted, patients might not see improvement for up to a year. Dr. Burns said that when he first learned medialization, he would go into the operating room (OR) with the skull base surgeon and do a permanent medialization before the tumor was resected, “just in anticipation that those nerves were going to go.” He said he prefers Gore-Tex, but there is flexibility. “Whatever solid material will support the paraglottic space is fine to put in there,” he said.