Separating the responders from the non-responders when it comes to surgery for obstructive sleep apnea (OSA) is a goal for all surgeons in this area, and a group of experts, focusing mostly on the role of the tongue in OSA, tackled the topic during a panel session.
Explore This Issue
March 2015“There is a variable response to UPPP [uvulopalatopharyngoplasty] and it’s important to determine what subgroup of the sleep apnea patients would benefit from surgery,” said Kathleen Yaremchuk, MD, MSA, chair of the department of otolaryngology at Henry Ford Health System in Detroit. The literature suggests that success rates with UPPP might be 50% or less over the long term.
Eric Kezirian, MD, MPH, professor of otolaryngology-head and neck surgery at Keck School of Medicine at the University of Southern California in Los Angeles, emphasized that advancements in evaluation techniques have shown that the tongue can play a major role in OSA but that other structures may contribute to airway obstruction.
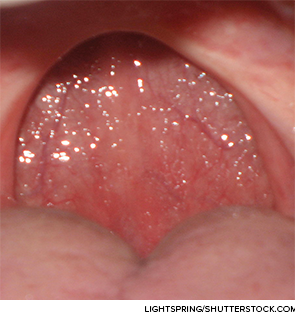
Techniques such as Friedman staging—which defines categories based on the size of the tongue and the size of the tonsils—can be useful as a first step because “it is associated with outcomes after UPPP with tonsillectomy,” he said. Those with large tonsils but relatively small tongues tend to do well, but those with large tongues tend to experience worse outcomes.
Drug-induced sleep endoscopy is another OSA evaluation technique that is based on fiberoptic examination of the airway under sedation. Dr. Kezirian’s research has shown the importance of the palate, oropharyngeal lateral walls, tongue, and epiglottis. One study of 33 patients who experienced persistent OSA after palate surgery showed that “almost all of them had obstruction related to the tongue, but that the other structures also contributed in many patients.”
From the audience
We’ve all had those patients who are not improving with our upper airway surgical techniques. And I’ve done base of tongue surgery and palatal surgery, and so I think [Inspire] is going to be one more treatment option for those who aren’t responders.
—Doug Anderson, MD, Ogden Clinic, Utah
Ho-Sheng Lin, MD, professor of otolaryngology-head and neck surgery at Wayne State University in Detroit, said that airway obstruction can be multi-layered and that this can sometimes be missed. “A failure to recognize the multi-level nature of airway obstruction may account for the poor surgical outcomes following UPPP,” he said.